Tetralogy of Fallot(TOF) is classically described as a variably cyanotic lesion consisting of right ventricular outflow tract obstruction, VSD, overriding aorta, and right ventricular hypertrophy. This tetralogy can be simplified, as was suggested by Van Pragh, to primary underdevelopment of the infundibulum of the right ventricular outflow including the pulmonary valve resulting in anterior, superior displacement of both the infundibular or conal septum and the aorta producing right ventricular outflow tract (RVOT) obstruction and aortic override1. Right ventricular hypertrophy develops as a consequence of unrelieved RVOT obstruction1.
This classic form of TOF is commonly called TOF with pulmonary stenosis (TOF/PS). The other forms of TOF are TOF with pulmonary atresia (TOF/PA) and TOF with absent pulmonary valve (TOF/APV).A subset of patients with TOF/PA have associated major aortopulmonary collaterals (MAPCAs) as an alternative source of pulmonary blood flow. We will focus on the perioperative imaging and decision making in TOF/PS.
Perioperative Considerations
The majority of TOF/PS patients will be allowed to grow without surgical or catheter-based intervention until 2-4 months of age. The benefit of this approach is that the child is larger making surgery technically easier for the surgeon. It also allows the pulmonary vascular resistance (PVR) to fall such that after repair the hypertrophic RV with poor diastolic function does not have to overcome the secondary insult of high PVR. In situations where neonatal TOF repair is necessitated by recurrent cyanotic episodes the atrial septum is often fenestrated to allow a right to left “pop-off” to maintain cardiac output and prevent postoperative right ventricular failure at the expense of a lower arterial oxygen saturation.
There are several surgical techniques to alleviate the RVOT tract obstruction; recently efforts have been directed toward preservation of pulmonary valve function. At many institutions RVOT muscle bundles are resected and patches are placed above and, if needed, below the valve. The annulus/valve is then dilated with a balloon, under direct vision by the surgeon, up to a Z score of 0 for the patient’s size. In patients in whom the annulus is prohibitively small a transannular patch (TAP) is done with recognition that pulmonary regurgitation requiring later intervention will be induced. While the non-TAP approach is effective in reducing the incidence and severity of pulmonary regurgitation, there is potentially an increased incidence of residual RVOT obstruction compared to the traditional TAP repair making postoperative evaluation of the RVOT even more critical.
Preoperative Questions and Associated TEE Views
Ventricular septal defect and presence of additional ventricular septal defects
Mid Esophageal Long Axis View (~ 120 degrees)
Mid Esophageal Short Axis view (~ 60 degrees)
4 Chamber View Mid Esophageal View (TEE, 0 degrees)
Degree and location of right ventricular outflow tract obstruction
Mid Esophageal Short Axis RVOT View (~ 60 degrees angle)
Mid to deep transgastric RVOT View (60-90 degrees)
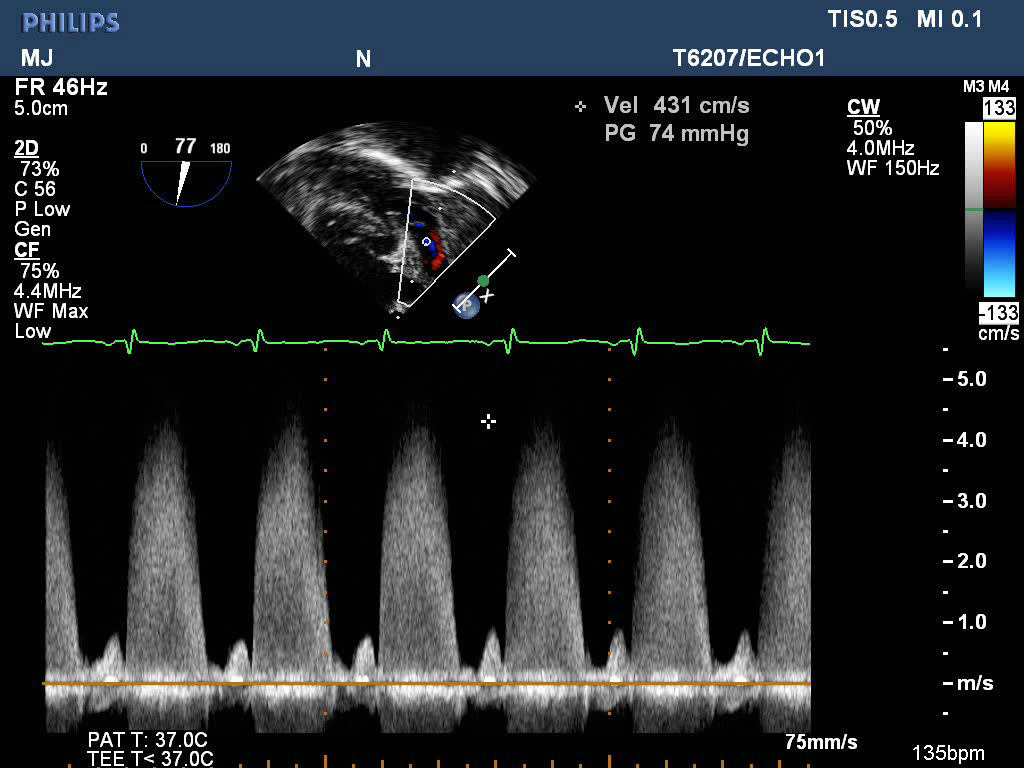
RVOT gradient
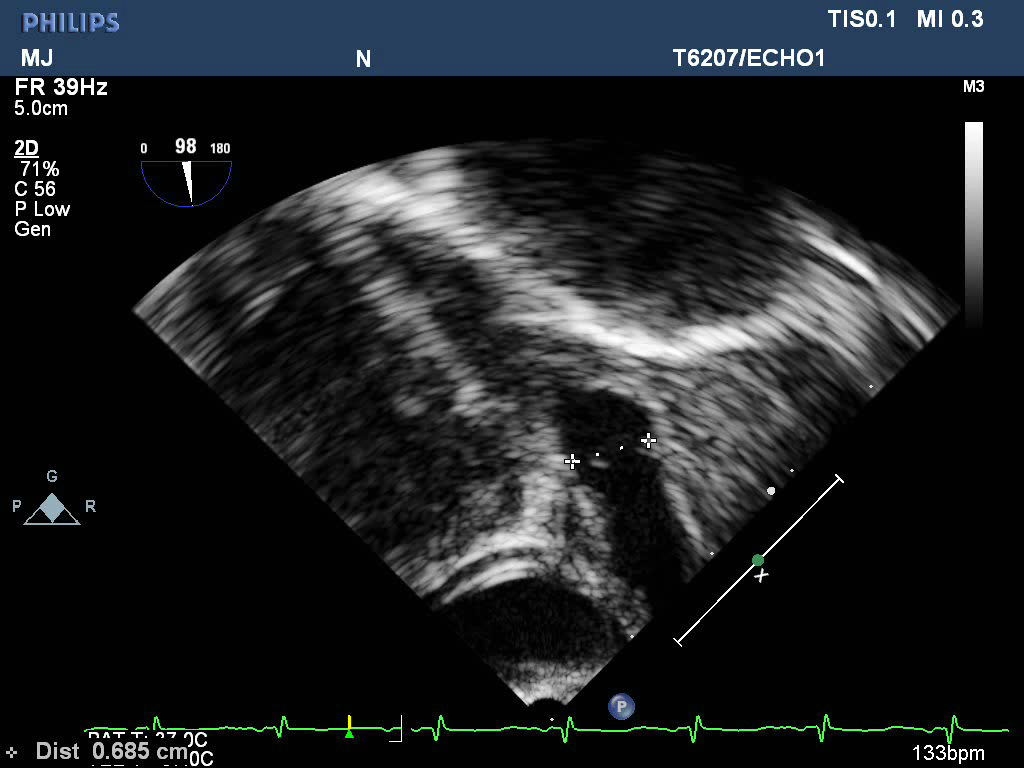
Pulmonary artery annulus dimension (to compare to images obtained by TTE for sizing of baloon)
Right coronary artery anatomy (if not clarified by TTE)
Transesophageal aortic short axis view (~ 30-45 degrees), just above the level of the aortic valve
Presence or absence of atrial septal communication
Midesophageal 4 chamber view, (0 degrees), rotated to left
Midesophageal bicaval view, (90 degrees)
Postoperative Questions and Associated TEE Views
Function
Midesophageal 4 Chamber (0 degrees)
Transgastric Short Axis (0 degrees)
RVOT Obstruction
Midesophageal short axis (60-90 degrees)
RVOT gradient
Mid to deep transgastric RVOT View (60-90 degrees)
Residual VSD
Midesophageal short axis (60-90 degrees)
Midesophageal 4 chamber (~0 degrees)
Midesophageal long axis (~ 120 degrees)
Presence or absence of atrial septal communication
Midesophageal 4 chamber view, (0 degrees), rotated to left
Midesophageal bicaval view, (90 degrees)
References
1. Van Praagh R: The first Stella van Praagh memorial lecture: the history and anatomy of tetralogy of Fallot. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 2009: 19-38