Author: Krupa Desai, MD – Children’s Hospital of Philadelphia; Chinwe Unegbu, MD – Children’s National Hospital
A three-year-old child with an atrial septal defect (ASD) presents for possible transcatheter ASD device closure. The interventional cardiologist plans on using intracardiac echocardiography (ICE) rather than transesophageal echocardiography (TEE). What represents the MOST LIKELY reason that ICE would be utilized for this procedure?
Correct!
Wrong!
Question of the Week 326
Transcatheter closure of an ASD represents a safe and effective alternative to surgical closure. Traditionally, imaging via transesophageal echocardiography (TEE) has been utilized to guide ASD closure. TEE has a well-established role in guiding interventional procedures due to its ability to provide real-time 3D imaging and superior image resolution when compared to transthoracic echocardiography. However, intracardiac echocardiography (ICE) is being used with increasing frequency and is replacing TEE as the primary imaging technique utilized to guide device closure of ASDs.
ICE is a unique imaging modality in that it can provide high-resolution real-time visualization of cardiac structures. ICE is typically performed with a catheter that is inserted through a venous sheath placed by the interventional cardiologist. The ICE catheter has an ultrasound transducer at its tip that emits sound waves to produce images of the heart. ICE allows for continuous monitoring of catheter location within the heart during a cardiac catheterization or electrophysiology study. As a result, early recognition of procedural complications, such as pericardial effusion or thrombus formation is possible. Additional benefits of ICE are excellent patient tolerance, reduction of fluoroscopy time, and lack of need for a second operator to acquire echocardiography images. In certain cases, general endotracheal anesthesia may be avoided if ICE is used instead of TEE, especially in adults. In the adult population, ICE has largely replaced TEE as the ideal imaging modality used to guide certain procedures, such as atrial septal defect closure and catheter ablation of cardiac arrhythmias. For adult electrophysiology studies, ICE has been widely adopted to guide transseptal punctures due to its ability to define atrial septal anatomy and provide visualization of transseptal catheter position in relation to other structures within the heart. ICE also has an emerging role in other catheter-based interventions.
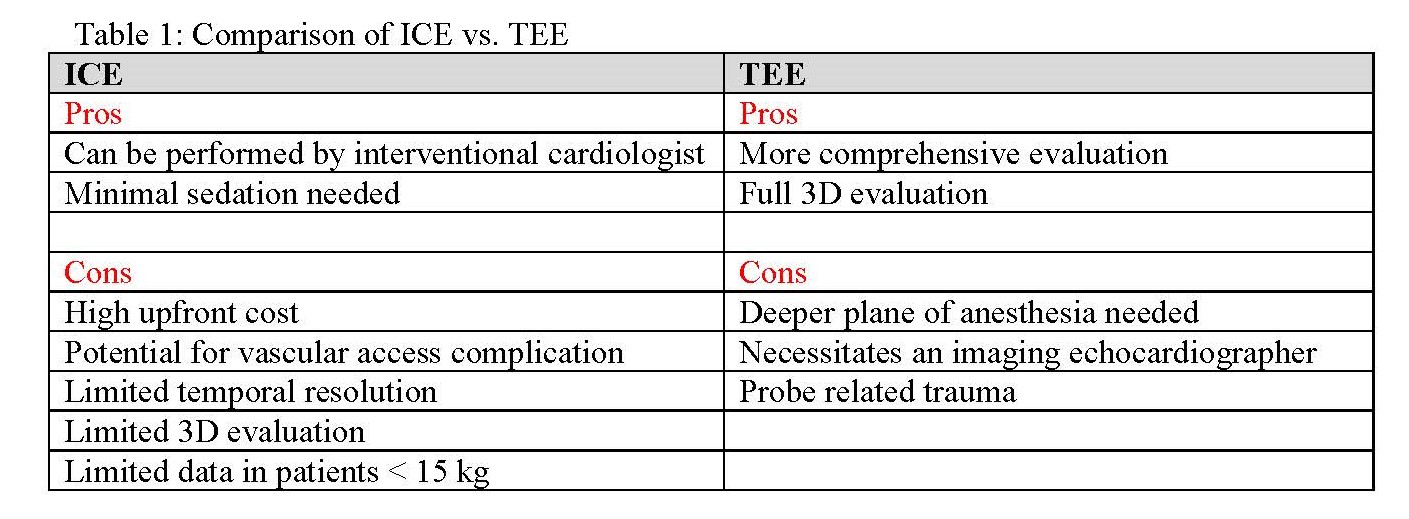
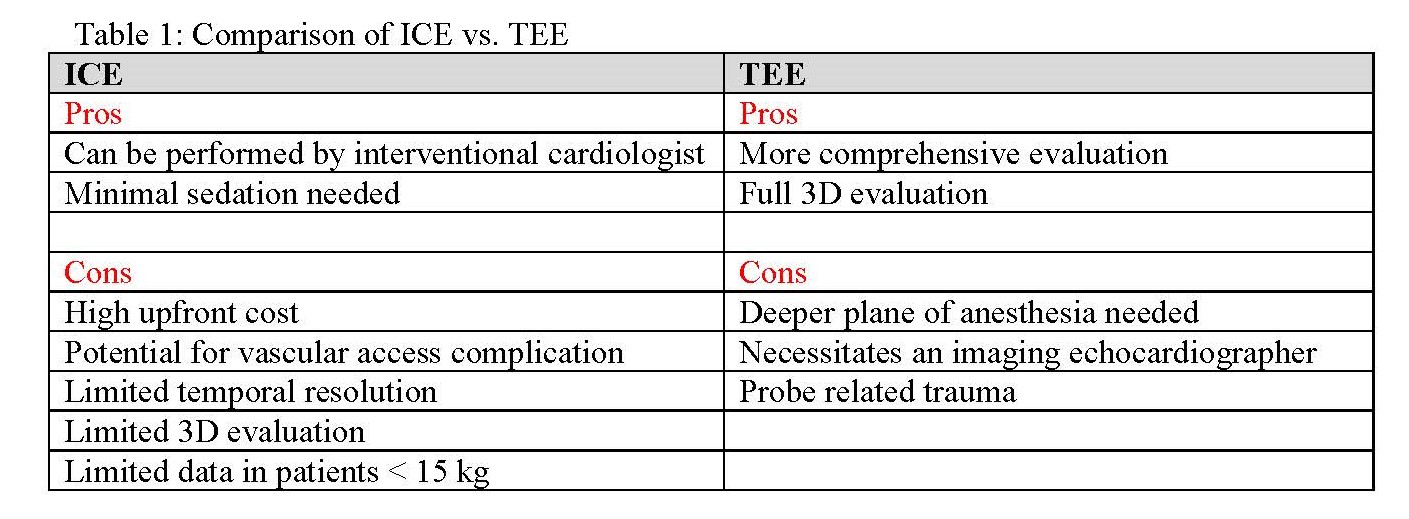
Both TEE and ICE have inherent strengths and weakness (see Table 1) that should be considered prior to deciding on the optimal imaging modality for a given procedure. ICE can be performed by the interventional cardiologist; therefore, a second operator isn’t needed for image acquisition. In pediatric centers that perform cardiac catheterization without intubation, ICE negates the need for a general endotracheal anesthetic. However, many institutions still perform general endotracheal anesthesia (GETA) for pediatric cardiac catheterizations. Therefore, the potential cost savings and patient comfort attributed to utilizing ICE may not be realized at those centers. Additionally, ICE generates images from within the heart at short distances with high spatial resolution. A critical role of ICE in the interventional cardiac catheterization lab is the early recognition of procedural complications. ICE allows for immediate assessment and differentiation of possible causes of hemodynamic compromise. Pericardial effusion is a serious complication of interventional cardiac catheterization procedures. ICE allows detection of pericardial effusion before the occurrence of hemodynamic changes.
Perceived disadvantages of ICE include the high upfront cost of the single-use catheters. There is also lower spatial resolution and image quality of far-field structures (from the right atrium) such as the pulmonary veins and left atrial appendage. Additionally, there is increased risk of vascular injury with insertion of the ICE catheter. Another major criticism of ICE is the limited number of published studies supporting its use in small children. Many published studies are either in adults or larger children. A study published by Patel et al in 2006 did demonstrate safety and efficacy of ICE to guide ASD device closure in patients smaller than 15 kg. Nonetheless, this remains an area of significant debate.
When compared to ICE, TEE has the advantage of lower upfront cost and does not require venous or arterial access thereby limiting vascular access-site complications. TEE also allows for more comprehensive cardiac imaging than with a full three dimensional (3D) evaluation. A known drawback with TEE is that it often requires GETA to facilitate placement of the TEE probe. Additionally, there is the chance for probe related trauma. Unlike ICE, which can be operated and interpreted by the interventional cardiologist, TEE requires an imaging echocardiographer. It is important to highlight that when necessary, both TEE and ICE, can be used in a complementary fashion. TEE can be used for initial evaluation and planning for ASD closure, and procedural ICE can provide additional guidance for device size selection and positioning.
References
1. Hijazi ZM, Wangt Z, Cao Q, et al. Transcatheter closure of atrial septal defects and patent foramen ovale under intracardiac echocardiographic guidance. Catheter Cardiovasc Interv. 2001; 52: 194–199.
2. Enriquez A, Saenz L, Rosso R, et al. Use of Intracardiac Echocardiography in Interventional Cardiology: Working with the Anatomy Rather Than Fighting It. Circulation. 2018; 137: 2278–2294.
3. Alqahtani F, Bhirud A, Aljohani S, et al. Intracardiac versus transesophageal echocardiography to guide transcatheter closure of interatrial communications: Nationwide trend and comparative analysis. J Interv Cardiol. 2017; 30: 234-241.
4. Basman C, Parmar Y, Kronzon I. Intracardiac Echocardiography for Structural Heart and Electrophysiological Interventions. Curr Cardiol Rep. 2017; 19: 102.
5. Assaidi A, Sumian M, Mauri L, et al. Transcatheter closure of complex atrial septal defects is efficient under intracardiac echocardiographic guidance. Arch Cardiovasc Dis. 2014; 107: 646-653.
6. Zanchetta M, Onorato E, Rigatelli G, et al. Intracardiac echocardiography-guided transcatheter closure of secundum atrial septal defect: A new efficient device selection method. J Am Coll Cardiol. 2003; 42: 1677–1682.
7. Patel A, Cao QL, Koenig P, Hijazi Z. Intracardiac echocardiography to guide closure of atrial septal defects in children less than 15 kilograms. Catheter and Cardiovasc Interv. 2006; 68: 287-291.
ICE is a unique imaging modality in that it can provide high-resolution real-time visualization of cardiac structures. ICE is typically performed with a catheter that is inserted through a venous sheath placed by the interventional cardiologist. The ICE catheter has an ultrasound transducer at its tip that emits sound waves to produce images of the heart. ICE allows for continuous monitoring of catheter location within the heart during a cardiac catheterization or electrophysiology study. As a result, early recognition of procedural complications, such as pericardial effusion or thrombus formation is possible. Additional benefits of ICE are excellent patient tolerance, reduction of fluoroscopy time, and lack of need for a second operator to acquire echocardiography images. In certain cases, general endotracheal anesthesia may be avoided if ICE is used instead of TEE, especially in adults. In the adult population, ICE has largely replaced TEE as the ideal imaging modality used to guide certain procedures, such as atrial septal defect closure and catheter ablation of cardiac arrhythmias. For adult electrophysiology studies, ICE has been widely adopted to guide transseptal punctures due to its ability to define atrial septal anatomy and provide visualization of transseptal catheter position in relation to other structures within the heart. ICE also has an emerging role in other catheter-based interventions.
Both TEE and ICE have inherent strengths and weakness (see Table 1) that should be considered prior to deciding on the optimal imaging modality for a given procedure. ICE can be performed by the interventional cardiologist; therefore, a second operator isn’t needed for image acquisition. In pediatric centers that perform cardiac catheterization without intubation, ICE negates the need for a general endotracheal anesthetic. However, many institutions still perform general endotracheal anesthesia (GETA) for pediatric cardiac catheterizations. Therefore, the potential cost savings and patient comfort attributed to utilizing ICE may not be realized at those centers. Additionally, ICE generates images from within the heart at short distances with high spatial resolution. A critical role of ICE in the interventional cardiac catheterization lab is the early recognition of procedural complications. ICE allows for immediate assessment and differentiation of possible causes of hemodynamic compromise. Pericardial effusion is a serious complication of interventional cardiac catheterization procedures. ICE allows detection of pericardial effusion before the occurrence of hemodynamic changes.
Perceived disadvantages of ICE include the high upfront cost of the single-use catheters. There is also lower spatial resolution and image quality of far-field structures (from the right atrium) such as the pulmonary veins and left atrial appendage. Additionally, there is increased risk of vascular injury with insertion of the ICE catheter. Another major criticism of ICE is the limited number of published studies supporting its use in small children. Many published studies are either in adults or larger children. A study published by Patel et al in 2006 did demonstrate safety and efficacy of ICE to guide ASD device closure in patients smaller than 15 kg. Nonetheless, this remains an area of significant debate.
When compared to ICE, TEE has the advantage of lower upfront cost and does not require venous or arterial access thereby limiting vascular access-site complications. TEE also allows for more comprehensive cardiac imaging than with a full three dimensional (3D) evaluation. A known drawback with TEE is that it often requires GETA to facilitate placement of the TEE probe. Additionally, there is the chance for probe related trauma. Unlike ICE, which can be operated and interpreted by the interventional cardiologist, TEE requires an imaging echocardiographer. It is important to highlight that when necessary, both TEE and ICE, can be used in a complementary fashion. TEE can be used for initial evaluation and planning for ASD closure, and procedural ICE can provide additional guidance for device size selection and positioning.
References
1. Hijazi ZM, Wangt Z, Cao Q, et al. Transcatheter closure of atrial septal defects and patent foramen ovale under intracardiac echocardiographic guidance. Catheter Cardiovasc Interv. 2001; 52: 194–199.
2. Enriquez A, Saenz L, Rosso R, et al. Use of Intracardiac Echocardiography in Interventional Cardiology: Working with the Anatomy Rather Than Fighting It. Circulation. 2018; 137: 2278–2294.
3. Alqahtani F, Bhirud A, Aljohani S, et al. Intracardiac versus transesophageal echocardiography to guide transcatheter closure of interatrial communications: Nationwide trend and comparative analysis. J Interv Cardiol. 2017; 30: 234-241.
4. Basman C, Parmar Y, Kronzon I. Intracardiac Echocardiography for Structural Heart and Electrophysiological Interventions. Curr Cardiol Rep. 2017; 19: 102.
5. Assaidi A, Sumian M, Mauri L, et al. Transcatheter closure of complex atrial septal defects is efficient under intracardiac echocardiographic guidance. Arch Cardiovasc Dis. 2014; 107: 646-653.
6. Zanchetta M, Onorato E, Rigatelli G, et al. Intracardiac echocardiography-guided transcatheter closure of secundum atrial septal defect: A new efficient device selection method. J Am Coll Cardiol. 2003; 42: 1677–1682.
7. Patel A, Cao QL, Koenig P, Hijazi Z. Intracardiac echocardiography to guide closure of atrial septal defects in children less than 15 kilograms. Catheter and Cardiovasc Interv. 2006; 68: 287-291.
