Author: Kevin Spellman, MD; Michael A. Evans, MD; Ann & Robert H. Lurie Children’s Hospital of Chicago, Northwestern Feinberg School of Medicine
A 5-month-old female infant with a history of congenital pulmonary valve stenosis status post transcatheter pulmonary valvuloplasty presents for surgical pulmonary valve repair due to residual stenosis with a peak gradient of 51 mmHg. In the operating room, a transannular patch is performed in addition to a commissurotomy secondary to the discovery of a bicuspid pulmonary valve with fused and thickened valve leaflets. Following separation from cardiopulmonary bypass, transesophageal echocardiography (TEE) demonstrates free pulmonary insufficiency in addition to the images illustrated below:
Based on the TEE findings, which of the following is the MOST appropriate course of clinical management?
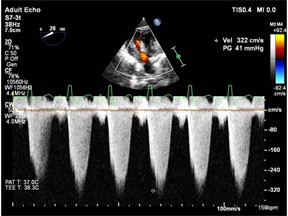
Image 1. Deep Transgastric RV Outflow Doppler Across Pulmonary Annulus
Clip 1. Mid Esophageal RV Inflow Outflow
EXPLANATION
Pulmonary valve stenosis can be present at the valve region (valvar), above the valve (supravalvar), or below the valve (subpulmonary/infundibular). Pulmonary valvar stenosis is graded based on the transpulmonary gradient, as planimetry is not possible given the available image planes. The pressure gradient is calculated based on the modified Bernoulli equation (∆P=4v2 ), which is dependent on the precision of the doppler measurements. If the ultrasound beam is not parallel to the direction of blood flow, velocity may be underestimated. The severity of pulmonary stenosis may also be graded by utilizing spectral doppler. Pulmonary stenosis is mild if the peak velocity is <3 m/s and peak gradient is 4 m/s and peak gradient >64 mmHg.
The question stem highlights a finding on the postoperative TEE of residual pulmonary valve stenosis. Clip #1 represents a Mid Esophageal RV Inflow Outflow View with the highest velocities measured near the pulmonary valve annulus. Continuous doppler over the pulmonary annulus (Image 1) demonstrates a peak velocity of 41 mmHg, which nearly matches the pre-operative value of 51 mmHg, and indicates that there is significant stenosis present despite surgery. Thus, in a patient who presented with symptomatic, moderate pulmonary stenosis while under general anesthesia (peak gradient of 51 mmHg) and had little improvement after the initial surgical repair (peak gradient of 41 mmHg) as illustrated by echo, the appropriate course of action is to reinitiate bypass and undergo further surgical intervention.
The surgeons must take down the transannular patch, and either 1) extend the ventriculotomy incision further into the right ventricular outflow tract or infundibulum thus revising the transannular patch or 2) resect the pulmonary valve. Often, extension of ventriculotomy and patch revision is limited by coronary anatomy. In this case, the question stem states that free pulmonary insufficiency is achieved, which in the setting of residual pulmonary stenosis indicates valve tissue and/or the small annulus continue to be obstructive. Thus, the correct answer is C, to resect the pulmonary valve. To avoid this complication, many surgeons resect pulmonary valve leaflets with the annular incision prior to sewing in the transannular patch.
Administration of protamine (answer A) would not be correct as there is a residual gradient requiring surgical correction.
The provided echocardiographic images do not indicate that right ventricular muscle bundles are responsible for residual stenosis (answer B), but rather that an area of stenosis at the level of the pulmonary valve is responsible.
REFERENCES
Baumgartner H, Hung J, Bermejo J, et al. Echocardiographic assessment of valve stenosis: EAE/ASE recommendations for clinical practice [published correction appears in Eur J Echocardiogr. 2009 May;10(3):479]. Eur J Echocardiogr. 2009;10(1):1-25. doi:10.1093/ejechocard/jen303
Linglart L, Gelb BD. Congenital heart defects in Noonan syndrome: Diagnosis, management, and treatment. Am J Med Genet C Semin Med Genet. 2020;184(1):73-80. doi:10.1002/ajmg.c.31765
Robertson M, Benson LN, Smallhorn JS, et al. The morphology of the right ventricular outflow tract after percutaneous pulmonary valvotomy: long term follow up. Br Heart J. 1987;58(3):239-244. doi:10.1136/hrt.58.3.239
Stout KK, Daniels CJ, Aboulhosn JA, et al. 2018 AHA/ACC Guideline for the Management of Adults With Congenital Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines [published correction appears in J Am Coll Cardiol. 2019 May 14;73(18):2361]. J Am Coll Cardiol. 2019;73(12):1494-1563. doi:10.1016/j.jacc.2018.08.1028
Waller BF, Howard J, Fess S. Pathology of pulmonic valve stenosis and pure regurgitation. Clin Cardiol. 1995;18(1):45-50. doi:10.1002/clc.4960180112
Puchalski MD, Lui GK, Miller-Hance WC, et al. Guidelines for Performing a Comprehensive Transesophageal Echocardiographic: Examination in Children and All Patients with Congenital Heart Disease: Recommendations from the American Society of Echocardiography [published correction appears in J Am Soc Echocardiogr. 2019 May;32(5):681] [published correction appears in J Am Soc Echocardiogr. 2019 Oct;32(10):1373-1378]. J Am Soc Echocardiogr. 2019;32(2):173-215. doi:10.1016/j.echo.2018.08.016
