Authors: Bryce Ferry, DO and Destiny F. Chau, MD - Arkansas Children’s Hospital/University of Arkansas for Medical Sciences, Little Rock, AR
A 3-month-old infant presenting with jaundice and pruritus undergoes liver biopsy which demonstrates multiple branches of the hepatic artery and vein and sparsity of bile ducts suggesting Alagille syndrome. What cardiac defect is MOST commonly associated with this syndrome?
EXPLANATION
Alagille syndrome is a rare inherited autosomal dominant disorder commonly associated with bile duct paucity, congenital cardiac defects and anomalies of other organs. It is associated with mutations in the JAG1 gene located on chromosome 20 (95%) or NOTCH2 gene located on chromosome 1 (5%). These mutations affect the notch signaling pathway leading to defective organogenesis and resulting in multiple systemic manifestations with a highly variable phenotype. This rare syndrome has an estimated prevalence of 1 in 70,000 newborns. De novo mutations account for half of the cases, with genetic inheritance accounting for the remainder.
The diagnostic criteria and major multi-system clinical manifestations are summarized in the table below, from Menon et al. (used under Creative Commons License).
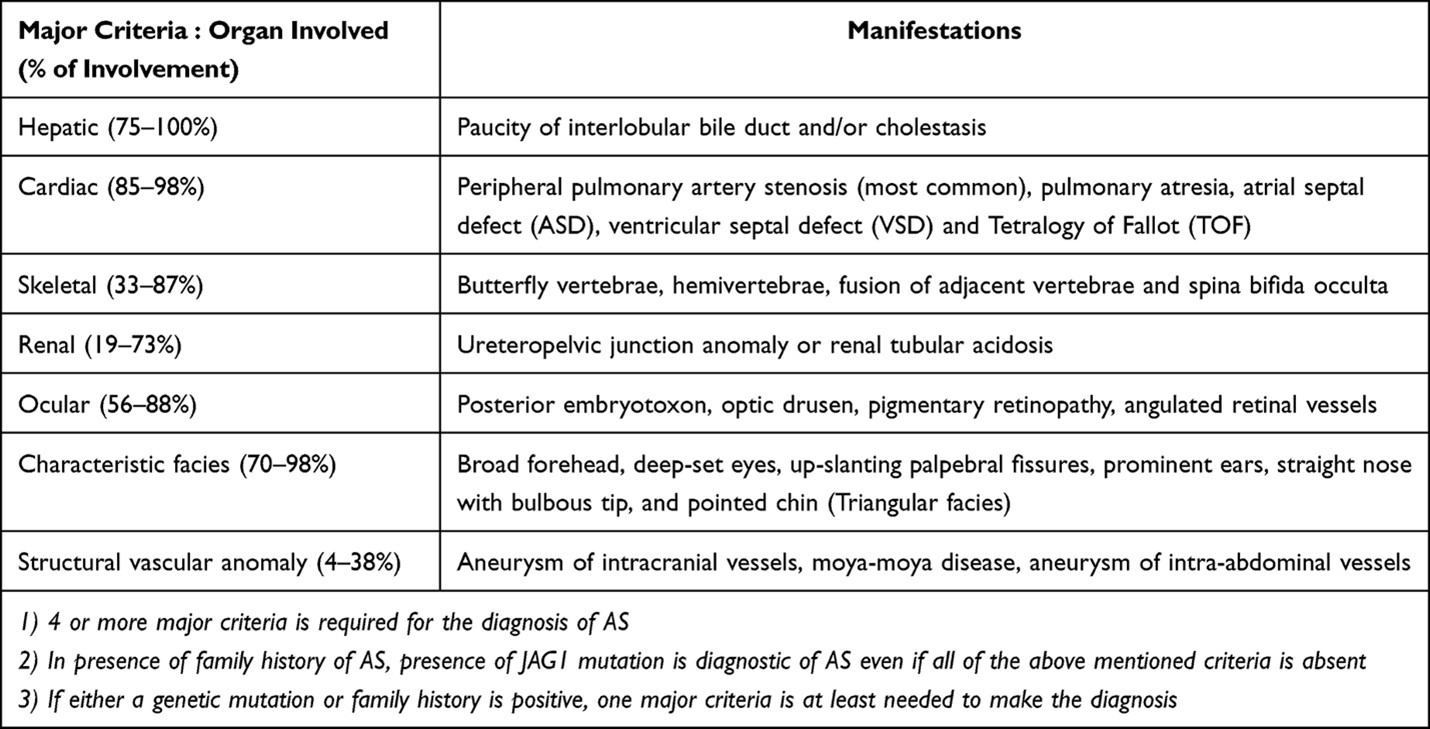 Diagnostic criteria for Alagille syndrome. From Menon et al. Multidisciplinary management of Alagille syndrome. J Multidiscip Healthc. 2022; 15:353-364. Used under Open Access Creative Commons License from Dove Press. (AS -Alagille Syndrome)
Diagnostic criteria for Alagille syndrome. From Menon et al. Multidisciplinary management of Alagille syndrome. J Multidiscip Healthc. 2022; 15:353-364. Used under Open Access Creative Commons License from Dove Press. (AS -Alagille Syndrome)
Congenital cardiac disease remains one of the primary causes of death. Emerick et al. studied 92 patients with Alagille syndrome and found the following causes of mortality: 15% from complex congenital heart disease, 25% from intracranial hemorrhage, and 25% from hepatic disease or transplantation. Patients with structural intracardiac lesions had a 40% predicted probability of being alive at 20 years old as compared to 80% for those without intracardiac defects. As hepatic involvement can worsen over time, interventions to correct and manage cardiac lesions must be promptly addressed to minimize morbidity and mortality due to other systemic diseases.
Pulmonary hemorrhage is common in patients with Alagille syndrome undergoing cardiac catherization procedures. In a retrospective, single-institution study, Adamson et al. reported the outcomes of 87 cardiac catheterizations in 30 children with Alagille syndrome. A total of 37% had interventions on the branch pulmonary arteries and 73% were diagnostic cardiac catheterizations. The study demonstrated that 44% (14 of 32) of interventional and 22% (12 of 55) of diagnostic catheterizations were complicated by pulmonary hemorrhage; the coagulation profiles and liver function tests were similar in those with and without pulmonary hemorrhage. The etiology of pulmonary hemorrhage was unclear. Notably, the JAG1 gene mutation, which is present in the majority of patients with Alagille syndrome, is expressed in both the arterial endothelium and in megakaryocytes. The JAG 1 gene plays an important role in vascular development and normal hemostasis. Therefore, mutation of the JAG1 gene may be a major contributing factor to pulmonary hemorrhage. Other factors associated with pulmonary hemorrhage included diagnosis of Tetralogy of Fallot, greater right ventricular systolic pressure to aortic systolic pressure ratio, and procedural/surgical interventions on the branch pulmonary arteries. Sixty five percent of pulmonary hemorrhages were mild, 15% were moderate, 19% were severe. The authors recommended a high degree of vigilance for this complication.
Patients with Alagille syndrome present for a variety of diagnostic and surgical procedures including the Kasai operation, liver biopsy and liver transplantation. Therefore, a thorough preoperative evaluation, with particular attention to the hepatic and cardiovascular systems, is essential for perioperative management. Hepatic disease varies from intractable pruritus to advanced liver dysfunction requiring liver transplantation. Patients may present with hepatomegaly and splenomegaly secondary to portal hypertension. Liver function tests usually show elevated gamma glutamyl transpeptidase, bilirubin and prolonged PT/PTT. The associated splenomegaly can result in thrombocytopenia, which may increase the risk of bleeding. Anesthetic drugs and neuromuscular blocking agents with minimal hepatic metabolism or excretion should be considered for patients with hepatic dysfunction. As chronic cholestasis can lead to osteopenia and fractures of long bones in this patient population, additional patient positioning precautions during general anesthesia are important. The presence of facial dysmorphism and vertebral anomalies are indicators of potential difficulty with mask ventilation and airway management. Associated cardiac lesions warrant appropriate anesthetic considerations tailored to the specific cardiac defect.
Peripheral pulmonary artery stenosis is the most common cardiac defect found in patients with Alagille syndrome. Hypoplastic left heart syndrome and common atrioventricular canal are not typically associated with this syndrome.
REFERENCES
Menon J, Shanmugam N, Vij M, Rammohan A, Rela M. Multidisciplinary management of Alagille syndrome. J Multidiscip Healthc . 2022;(15):353-364. doi:10.2147/JMDH.S295441
Yildiz T, Yumuk N, Baykal D, Solak M, Toker K. Alagille syndrome and anesthesia management. Pediatr Anesth . 2007; 87-97 doi:10.1111/j.1460-9592.2006.02022.x
Emerick KM, Rand EB, Goldmuntz E, Krantz ID, Spinner NB, Piccoli DA. Features of Alagille syndrome in 92 patients: frequency and relation to prognosis. Hepatology. 1999;29(3):822-829. doi:10.1002/hep.510290331
Mitchell E, Gilbert M, Loomes KM. Alagille Syndrome. Clin Liver Dis .2018;22(4):625-641. doi:10.1016/j.cld.2018.06.001
Adamson GT, Peng LF, Feinstein JA, et al. Pulmonary hemorrhage in children with Alagille syndrome undergoing cardiac catheterization. Catheter Cardiovasc Interv. 2020;95(2):262-269. doi:10.1002/ccd.28508
