Author: Meera Gangadharan, MD, FASA, FAAP - University of Texas at Houston, McGovern Medical School, Children’s Memorial Hermann Hospital
A 5-year-old male with a history of Tetralogy of Fallot presents for revision of a right ventricle to pulmonary artery conduit. A multi-modal plan for post-operative pain control includes regional anesthesia. Which of the following regional techniques is MOST likely to provide the best post-operative analgesia in this patient?
EXPLANATION
Effective pain control after pediatric cardiac surgery is essential for enhanced recovery protocols. These protocols include early extubation, rapid mobilization, reduction in opioid use to minimize side effects, and shortened intensive care unit and hospital stay. Recent trends recommend multimodal approaches to pain management, including regional anesthetic techniques, to reduce systemic opioid use. Neuraxial techniques for pain control are not widely utilized in pediatric cardiac surgery due to the potential risk of bleeding from heparinization during cardiopulmonary bypass. However, there are several peripheral nerve blocks (musculofascial plane blocks), which are efficacious in a multimodal analgesic regimen after pediatric cardiac surgery.
The target of a peripheral nerve block for a median sternotomy or intercostal incision is the anterior/ventral division of the spinal cord, which is the intercostal nerve. Intercostal nerves arise from the anterior rami of the thoracic spinal nerves and lie in between the innermost and internal intercostal muscles. Along its course from the spinal cord, the intercostal nerve branches into collateral and lateral cutaneous branches and finally terminates in the anterior cutaneous branch, which is distributed along the lateral and anterior chest wall. These branches provide sensory innervation to the skin, soft tissue, and muscle on the anterior aspect of the trunk, including the sternum. Thus, blocking the intercostal nerve at any reasonable site is the basis for a peripheral nerve block for cardiac surgery with a median sternotomy or intercostal incision.
Intercostal muscles lie between the ribs. The pectoralis major muscle overlies the ribs. The intercostal muscles consist of three layers: the external, internal, and innermost intercostal muscles. The intercostal vessels are located on the lower margin of the ribs in the layer between the internal and innermost intercostal muscles. The transverse thoracic muscle lies below the innermost intercostal muscle and may be difficult to identify. The pleura lies below the intercostal muscles and can be identified as a mobile hyperechoic layer.
The intercostal nerves arising from the ventral rami of the first six thoracic spinal nerves, supply the sternum, ribs, and intercostal sites. Effective pain relief for a sternotomy or intercostal incision can be provided by blocking the intercostal nerves anywhere along their path (see illustration below). A bilateral parasternal block (PSB) can be performed by the surgeon under direct vision by injecting local anesthetic at a point that is 1.5 to 2 cm lateral to the sternum at the second to sixth intercostal spaces. The PSB has been shown to reduce opioid requirements in the first 24 hours and lower pain scores in pediatric patients after cardiac surgery.
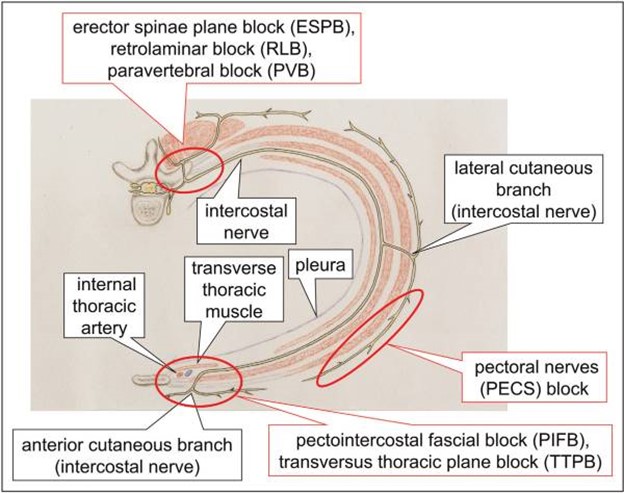
Fig. Schema of access points to the intercostal nerve blocks for perioperative pain management for cardiac surgery. Blocking the intercostal nerve at any approachable site is the theory of peripheral nerve block for cardiac surgery with median sternotomy as well as intercostal approach. From: Yamamoto T, Schindler E. Regional anesthesia as part of enhanced recovery strategies in pediatric cardiac surgery. Curr Opin Anaesthesiol. 2023;36(3):324-333. doi:10.1097/ACO.0000000000001262. This is an open access article distributed under the terms of the Creative Commons Attribution-Non Commercial-No Derivatives License 4.0 (CCBY-NC-ND), where it is permissible to download and share the work provided it is properly cited. The work cannot be changed in any way or used commercially without permission from the journal. http://creativecommons.org/licenses/by-nc-nd/4.0
A major disadvantage of the PSB is that multiple injections are required as the target intercostal nerves lie in the layer between the internal intercostal and innermost intercostal muscles, in the intercostal space. Two musculofascial plane blocks are alternative approaches to the parasternal block, which include the pectointercostal fascial block (PIFB) and transversus thoracic plane block (TTPB). Local anesthetic can thus spread along the fascial layers between muscles to cover multiple intercostal levels. Ultrasound guided PIFB and TTPB can be accomplished in the supine position. Local anesthetic is injected between the pectoralis major and the intercostal muscle layer in the PIFB. In the TTPB block, local anesthetic is injected between the innermost intercostal muscle and the transversus thoracic muscle. The PIFB has been reported to reduce opioid requirements and postoperative pain in the first 24 hours after surgery, as well as reducing the time to extubation and length of hospital stay. A retrospective study in pediatric patients demonstrated reduced intra and postoperative fentanyl use, postoperative pain scores and time to extubation. The PIFB and TTPB fascial block do not cover chest tube sites in the upper abdomen. Therefore, a rectus sheath block (RSB) is a useful adjunct to provide adequate analgesia after cardiac surgery. The efficacy of combining a RSB on the side ipsilateral to the chest tube and bilateral PIFBs has recently been described in pediatric patients after cardiac surgery in a retrospective, single center study. In this study, these interventions were associated with decreases in postoperative opioid use, pain scores and hospital length of stay.
The pectoral nerves blocks (PECS 1 and PECS 2) anesthetize the pectoral nerves, the third through sixth intercostal nerves, intercostobrachial nerve, and the long thoracic nerve. These blocks are performed by depositing local anesthetic between the pectoralis minor and major muscles (PECS 1) and between pectoralis minor and serratus anterior (PECS 2) muscles respectively. These blocks are more effective for surgical incisions that are further from the midline such as thoracotomy incisions and incisions for pacemaker implantations and breast surgery, but they are inadequate for a midline sternotomy incision.
The transversus abdominis plane block is inadequate for sternotomy and upper abdominal midline pain but is useful for procedures with lower abdominal incisions.
REFERENCES
Yamamoto T, Schindler E. Regional anesthesia as part of enhanced recovery strategies in pediatric cardiac surgery. Curr Opin Anaesthesiol. 2023;36(3):324-333. doi:10.1097/ACO.0000000000001262
Raj N. Regional anesthesia for sternotomy and bypass-Beyond the epidural. Paediatr Anaesth. 2019;29(5):519-529. doi:10.1111/pan.13626
Chaudhary V, Chauhan S, Choudhury M, et al. Parasternal intercostal block with ropivacaine for postoperative analgesia in pediatric patients undergoing cardiac surgery: a double-blind, randomized, controlled study. J Cardiothorac Vasc Anesth .2012; 26:439–442
Bloc S, Perot BP, Gibert H, et al. Efficacy of parasternal block to decrease intraoperative opioid use in coronary artery bypass surgery via sternotomy: a randomized controlled trial. Reg Anesth Pain Med. 2021;46(8):671-678. doi:10.1136/rapm-2020-102207
Fuller S, Kumar SR, Roy N, et al. The American Association for Thoracic Surgery Congenital Cardiac Surgery Working Group 2021 consensus document on a comprehensive perioperative approach to enhanced recovery after pediatric cardiac surgery. J Thorac Cardiovasc Surg .2021;162(3):931-954. doi:10.1016/j.jtcvs.2021.04.072
Tran DQ, Bravo D, Leurcharusmee P, Neal JM. Transversus Abdominis Plane Block: A Narrative Review. Anesthesiology. 2019;131(5):1166-1190. doi:10.1097/ALN.0000000000002842
Kumar AK, Chauhan S, Bhoi D, Kaushal B. Pectointercostal fascial block (PIFB) as a novel technique for postoperative pain management in patients undergoing cardiac surgery. J Cardiothorac Vasc Anesth .2021; 35:116–122.
Zhang Y, Gong H, Zhan B, Chen S. Effects of bilateral Pecto-intercostal Fascial Block for perioperative pain management in patients undergoing open cardiac surgery: a prospective randomized study. BMC Anesthesiol. 2021; 21:175.
Einhorn LM, Andrew BY, Nelsen DA, Ames WA. Analgesic effects of a novel combination of regional anesthesia after pediatric cardiac surgery: a retrospective cohort study. J Cardiothorac Vasc Anesth. 2022; 36:4054–4061.
Cakmak M, Isik O. Transversus thoracic muscle plane block for analgesia after pediatric cardiac surgery. J Cardiothorac Vasc Anesth. 2021; 35:130–136
