Author: Meera Gangadharan, MD, FASA, FAAP - University of Texas at Houston, McGovern Medical School, Children’s Memorial Hermann Hospital
A 2.5-year-old male with history of hypoplastic left heart syndrome palliated with a bidirectional Glenn is undergoing a pre-Fontan cardiac catheterization. Pertinent catheterization findings include a systemic arterial saturation (SaO2) of 73%, Qp:Qs of 0.8, and pulmonary vascular resistance (PVR) of 2.6 international woods units (iWU). Which of these hemodynamic variables is associated with the HIGHEST periprocedural risk of adverse event(s)?
EXPLANATION
Risk-stratification has become an important component of perioperative planning.. Procedural risk is the sum of the risk of the procedure and the risk imposed by the physiologic condition of the patient. Cardiac catheterization in patients with congenital heart disease is an evolving field with new procedures and technologies being developed and utilized in clinical practice.
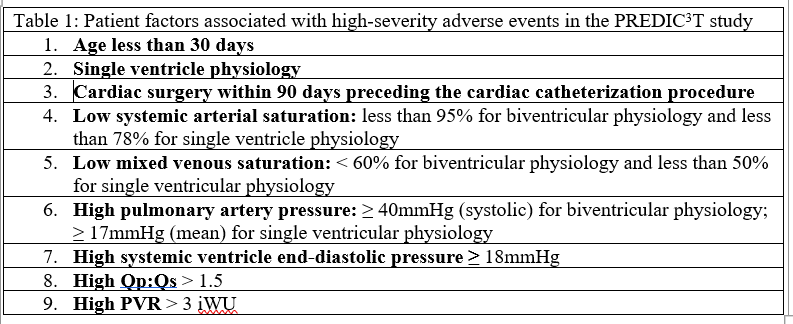
The 2022 Procedural Risk in Congenital Cardiac Catheterization (PREDIC3T) study by Quinn and colleagues was used to create a risk assessment tool for pediatric cardiac catheterization procedures. In this study, data from 23,119 pediatric and adult congenital cardiac catheterization cases between January 2014 and January 2018 were analyzed from 13 centers in the United States. Electrophysiological studies were excluded. The primary outcome was the occurrence of a clinically significant adverse event or a high severity adverse event (HSAE). Levels of adverse event severity were graded from zero to five, based on previously established definitions. Levels one and two were none/minor. Level three was a moderate severity event that resulted in a transient change in the patient’s condition that may have been life-threatening if not treated, required additional medications or transfer to an ICU. Examples include unstable arrythmias with stable blood pressure but requiring intervention, or vascular damage that was not life threatening but required intervention. Level four was a major event that was life-threatening or required cardiopulmonary resuscitation or emergent surgical intervention. Level five was a catastrophic event needing heart-lung support with failure to wean from such support and resulting in death. For this study, levels three through five were considered HSAEs. The study demonstrated that an adverse event occurred in 10.9% of cases and a high severity adverse event (HSAE) occurred in 5.2% of cases. Patient factors that were associated with high-severity adverse events (HSAEs) listed in table 1.
Cases or procedures were also divided into six risk categories from zero to five (see Table 2). The risk category was an independent predictor of increased risk of HSAEs, with odds-ratios ranging from zero for risk category zero, to 5.25 for risk category five (p ≤ 0.005).
Table 2: PREDIC3 T Case-Type Risk Categories
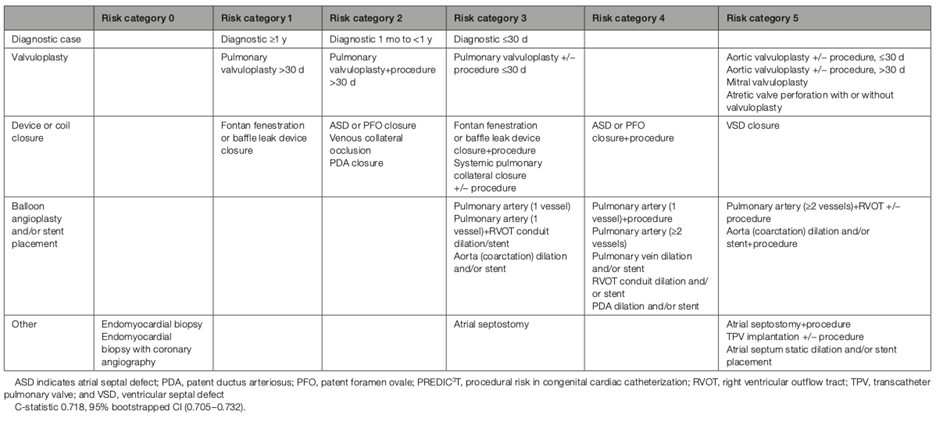 Table from: Quinn BP, Yeh M, Gauvreau K, et al. Procedural Risk in Congenital Cardiac Catheterization (PREDIC3T). J Am Heart Assoc. 2022;11(1):e022832. Used under Creative Commons License.
Table from: Quinn BP, Yeh M, Gauvreau K, et al. Procedural Risk in Congenital Cardiac Catheterization (PREDIC3T). J Am Heart Assoc. 2022;11(1):e022832. Used under Creative Commons License.
Additional scoring systems have been developed to quantify risk in cardiac catheterization procedures. In a 2016 study by Nykanen and colleagues, the Congenital Cardiac Interventional Study Consortium developed the Catheterization Risk Score for Pediatrics (CRISP) to predict the likelihood of serious adverse events occurring during cardiac catheterization. The factors included age, weight, inotropic support, organ failure, physiologic category, diagnosis, procedure category and procedure type (diagnostic, interventional or hybrid). The physiologic category was based on systemic saturation, indexed pulmonary vascular resistance, right ventricular systolic pressure /systemic pressure ratio, anemia, right ventricular outflow obstruction and systemic atrio-ventricular valve regurgitation. Five risk scores were defined: with a CRISP score of five being the highest risk and CRISP score of one being the lowest risk for serious adverse events.
These various risk-assessment tools can also be useful for resource allocation during perioperative planning. A multispecialty society expert consensus statement published in 2016 by Odegard and colleagues offers guidance for pediatric cardiac catheterization procedures. The authors state that a pediatric cardiac anesthesiologist should provide care for patients presenting with a CRISP score equal to or greater than five. Anesthesiologists with a “special expertise” in congenital heart disease should provide care for patients with a CRISP score between two and four, and the sedation team can provide care for patients with a CRISP score of zero to one.
Based on the PREDIC3T project, for single ventricle patients, a systemic arterial oxygen saturation below 78% increases the risk of experiencing a HSAE. A Qp:Qs of less than 1.5 and a PVR < 3iWU does not increase the risk of a HSAEs.
REFERENCES
Nykanen DG, Forbes TJ, Du W, et al. CRISP: Catheterization RISk score for Pediatrics: A Report from the Congenital Cardiac Interventional Study Consortium (CCISC). Catheter Cardiovasc Interv. 2016;87(2):302-309. doi:10.1002/ccd.26300
Quinn BP, Yeh M, Gauvreau K, et al. Procedural Risk in Congenital Cardiac Catheterization (PREDIC3T). J Am Heart Assoc. 2022;11(1):e022832. doi:10.1161/JAHA.121.022832
Odegard KC, Vincent R, Baijal RG, et al. SCAI/CCAS/SPA Expert Consensus Statement for Anesthesia and Sedation Practice: Recommendations for Patients Undergoing Diagnostic and Therapeutic Procedures in the Pediatric and Congenital Cardiac Catheterization Laboratory. Anesth Analg. .2016;123(5):1201-1209. doi:10.1213/ANE.0000000000001608
