Authors: Manal Mirreh, MD AND Divya Madhusudhan, MD - Children’s Hospital of Philadelphia, Philadelphia, PA
A 6-month-old, 5 kg girl with history of severe biventricular dysfunction secondary to perinatal myocardial infarction managed initially with VA ECMO and now supported with Berlin VAD is awaiting heart transplantation. Which of the following patient characteristics is associated with the BEST long-term survival after pediatric heart transplantation?
EXPLANATION
Significant advancements in anesthetic management, immunosuppression and postoperative management have improved outcomes in pediatric heart transplant recipients, with 1 year survival rates now over 90%.
According to data from the International Society of Heart and Lung Transplantation ISHLT), leading causes of early mortality are graft failure, acute rejection, coronary artery vasculopathy and infection.
The Kaplan-Meier survival curves for patients of differing ages after transplant are presented below (Figure 1). The youngest recipients have the longest median survival to 24.5 years; however, infants are also at the highest risk of dying in the early period post-transplant.1
Figure 1: Kaplan-Meier Survival Curve from ISHLT
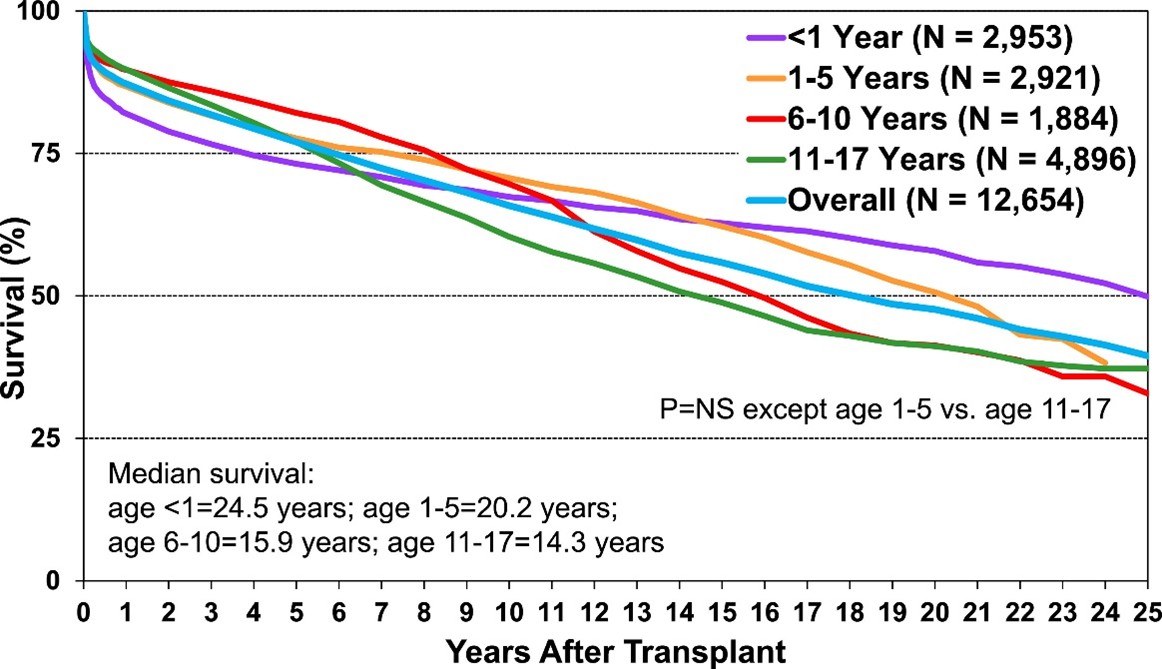 Kaplan-Meier survival curve generated from the International Society of Heart and Lung Transplantation (J Heart Lung Transplant. 2019;38(10):1028-1041. DOI: 10.1016/j.healun.2019.08.002)
This work is openly licensed via CC BY 4.0.
Kaplan-Meier survival curve generated from the International Society of Heart and Lung Transplantation (J Heart Lung Transplant. 2019;38(10):1028-1041. DOI: 10.1016/j.healun.2019.08.002)
This work is openly licensed via CC BY 4.0.
There is an inverse relationship between age at transplant and survival.
A study in Circulation reported that the actuarial survival after infant heart transplantation was 84% at 1 month and 70% at 1 year with greatest hazard for death occurring within the first 3 months.2
Diagnosis of cardiomyopathy (especially dilated cardiomyopathy) is associated with better outcomes than congenital heart disease, especially those with complex anatomy or multiple prior surgeries.
Patients transplanted while on ECMO support had significantly decreased survival post-transplant compared with patients on VAD support or no mechanical support.3
REFERENCES
1. Rossano JW, Singh TP, Cherikh WS, et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: Twenty-second pediatric heart transplantation report - 2019; Focus theme: Donor and recipient size match. J Heart Lung Transplant. 2019;38(10):1028-1041. doi:10.1016/j.healun.2019.08.002
2. Canter C, Naftel D, Caldwell R, et al. Survival and risk factors for death after cardiac transplantation in infants. A multi-institutional study. The Pediatric Heart Transplant Study. Circulation. 1997;96(1):227-231. doi:10.1161/01.cir.96.1.227
3. Conway J, Cantor R, Koehl D, et al. Survival After Heart Transplant Listing for Infants on Mechanical Circulatory Support [published correction appears in J Am Heart Assoc. 2020 Dec 15;9(24):e014641. doi: 10.1161/JAHA.119.014641.].
