Authors: Manal Mirreh, MD, Jennifer M. Lynch, MD, PhD, Lea C. Matthews, MD – Children’s Hospital of Philadelphia, Philadelphia, PA
A 4-day-old, 3 kg neonate with HLHS is undergoing a Norwood procedure under hypothermic cardiopulmonary bypass. A few minutes after initiation of antegrade cerebral perfusion (ACP) through the innominate artery, a decrease in bilateral cerebral NIRS values is observed. Which of the following is the MOST LIKELY explanation for the observed drop?
EXPLANATION
Near-infrared spectroscopy (NIRS) offers continuous, non-invasive monitoring of regional tissue oxygen saturation (rSO2), reflecting the balance between oxygen delivery and consumption at the tissue level. The NIRS value represents the relative ratio of hemoglobin that remains oxygenated after traversing the local tissue bed. Trending NIRS values can help detect fluctuations in oxygen delivery and/or utilization.
NIRS is based on the modified Beer-Lambert Law, which describes how light travels through a scattering medium. NIRS emits near-infrared light through tissues and measures the amount of light at different wavelengths absorbed by oxygenated and deoxygenated hemoglobin. From this information, regional oxygen saturation (rSO2) can be calculated.1
Tissue oxygenation is related to oxygen delivery to the tissue (i.e., arterial oxygen content and blood flow) and oxygen consumption by the tissue. Thus, rSO2 fluctuates as these parameters change.
Clinically used conventional continuous-wave near-infrared spectroscopy (NIRS) has several limitations that should be considered when interpreting its readings. First, its spatial coverage is limited, as it primarily monitors the superficial anterior brain regions where the sensors are placed—typically the frontal cortex—potentially missing injuries in deeper or posterior areas such as the parieto-occipital regions. Additionally, NIRS provides relative rather than absolute values, which makes clinical guidelines based on absolute rSO2 values hard to establish. Furthermore, its accuracy as even a relative trend monitor can be limited depending on factors such as hemoglobin concentration and temperature changes2, which is a crucial point, particularly in this patient population, due to the widespread use of hypothermic cardiopulmonary bypass.3
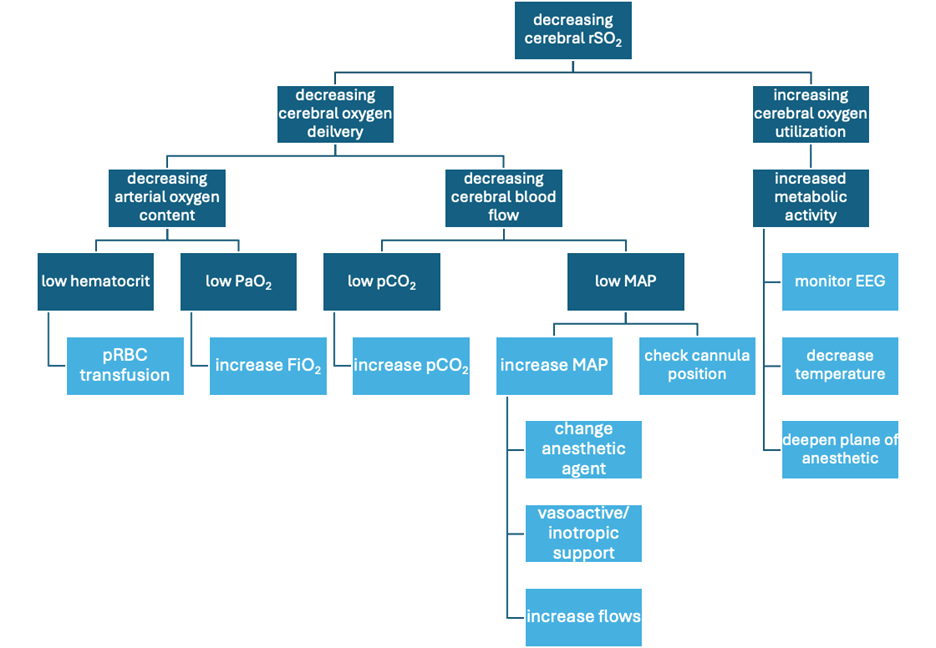
Below is a suggested decision tree guiding management when decreasing cerebral rSO2 on CPB is encountered:
A Circle of Willis (cerebral circulation) abnormality (Answer A) would result in an asymmetric drop in rSO2 during antegrade cerebral perfusion due to inadequate blood flow to the contralateral brain. It would not result in bilateral drops in cerebral rSO2, assuming adequate flow rate and unimpinged cerebral venous return.
Changes in temperature do affect rSO2 values as cerebral metabolic rate changes. However, periods of antegrade cerebral perfusion typically occur during deep hypothermia, which aims to reduce cerebral metabolic rate. Thus, an increase in cerebral demand due to hypothermia (Answer C) is incorrect.
There are many reasons that bilateral cerebral NIRS values may drop during the course of cardiopulmonary bypass, including low hematocrit, arterial cannula malposition, or obstruction to venous drainage. However, of the choices presented, only inadequate flow (Answer B) represents a possible explanation in this case.
REFERENCES
1. Owen-Reece H, Smith M, Elwell CE, Goldstone JC. Near infrared spectroscopy. Br J Anaesth. 1999;82(3):418-426. doi:10.1093/bja/82.3.418
2. Kleiser S, Ostojic D, Andresen B, et al. Comparison of tissue oximeters on a liquid phantom with adjustable optical properties: an extension. Biomed Opt Express. 2017;9(1):86-101. Published 2017 Dec 5. doi:10.1364/BOE.9.000086
3. Lynch JM, Mavroudis CD, Ko TS, et al. Association of Ongoing Cerebral Oxygen Extraction During Deep Hypothermic Circulatory Arrest With Postoperative Brain Injury. Semin Thorac Cardiovasc Surg. 2022;34(4):1275-1284. doi:10.1053/j.semtcvs.2021.08.026
