Contributors: Wanda C. Miller-Hance, MD and Pablo Motta, MD; Texas Children’s Hospital and Baylor College of Medicine, Houston, TX Overview
The bicuspid aortic valve (BAV) is the most common congenital cardiac malformation with a prevalence between 1 to 2% of the general population. A known male predominance is recognized as well as a familial occurrence. This is the most common lesion that affects the aortic valve (AV). The anomaly can present as an incidental finding on echocardiography, in fact, many children with BAV disease are completely asymptomatic. Potential problems, affecting nearly a third of patients, include aortic valve stenosis, aortic regurgitation, infective endocarditis, and aortic root dilation/aneurysm formation/aortic dissection/rupture. A BAV can develop progressive sclerosis and calcification resulting in stenosis later in life. Aortic dilation can also develop over time, even in the absence of valvar stenosis. This has led to consideration of BAV disease as a genetic vasculopathy.
Several distinct anatomic types of BAV are identified; the most common form is characterized by fusion of the valvar leaflets along a commissure or underdevelopment in one of the commissures (raphe) resulting in a ‘functionally’ bileaflet valvar structure (bicommisural aortic valve) with unequal-sized leaflets. Less frequently in this lesion, only two well-developed, equal-sized leaflets are present (‘true’ bileaflet or bicuspic valve).
A BAV can be found in isolation, however, it is frequently seen within the context of other congenital cardiovascular malformations (i.e., ventricular septal defect, aortic coarctation, interrupted aortic arch, Shone’s complex or related variants).
Transesophageal Echocardiography (TEE)
The AV anatomy is best displayed by TEE at the level of the mid-esophagus in the following views:
- Mid-esophageal aortic valve short-axis view (ME AV SAX): obtained with plane rotation to ~ 20-60°. In the normal AV three cusps are visualized in this view; the right coronary cusp is to the right (left of the display) and most anterior, the left coronary cusp is to the left (closer to the pulmonary artery, to the right of the display), and the noncoronary cusp is near the interatrial septum (closer to the narrowest portion of the sector). The cusps are normally symmetrical in size, of similar shape, and meet each other at the commissures during diastole.With respect to the BAV, this view allows for evaluation of valve morphology, fusion of commissures (most commonly the intercoronary commissure) and leaflet motion (fish-mouth appearance of valve orifice). This can be seen in Videos
and. Thickening, restricted motion and calcification are frequently observed in aortic stenosis. Lack of leaflet coaptation is associated with aortic regurgitation. Color Doppler can be applied to qualitatively examine the degree of turbulence and presence/site of regurgitation. In systole the AV orifice can be traced by planimetry to determine valve area, however, this measurement has a number of limitations and is not of much utility in the pediatric patient.
- Mid-esophageal aortic valve long-axis (ME AV LAX) and mid-esophageal long-axis (ME LAX) views: obtained with probe rotation to ~120-150°. These views allow for visualization of the left ventricular outflow tract, AV and ascending aorta. AV motion (eccentric closure and doming in the BAV) is well seen in these cross-sections
andVarious measurements can be obtained that include the aortic annulus (most proximal attachment of the semilunar valve), aortic root (portion between the aortic annulus and sinotubular junction), sino-tubular junction (region of the ascending aorta at superior portion of the aortic sinuses) and ascending aorta. Color Doppler can be applied to detect flow acceleration and/or regurgitant flow. These views cannot be used for quantitative Doppler since the cursor cannot be optimally aligned with the direction of blood flow.
Additional TEE views required for the quantitative evaluation of aortic stenosis and to facilitate the examination of aortic regurgitation include:
- Transgastric long-axis view (TG LAX): obtained by rotating the plane to ~120°
once the transgastric left ventricular short axis view is displayed
- Deep transgastric long-axis view (DTG LAX): obtained after the probe is advanced into the fundus of the stomach (~ 0 plane) and anteflexed or retroflexed as required until the AV comes into view
.
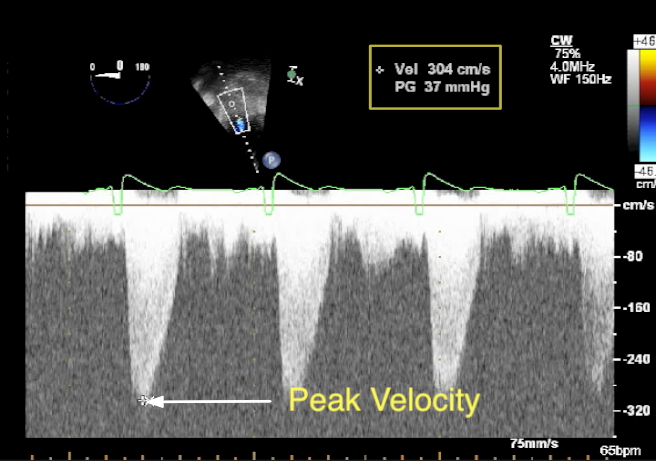
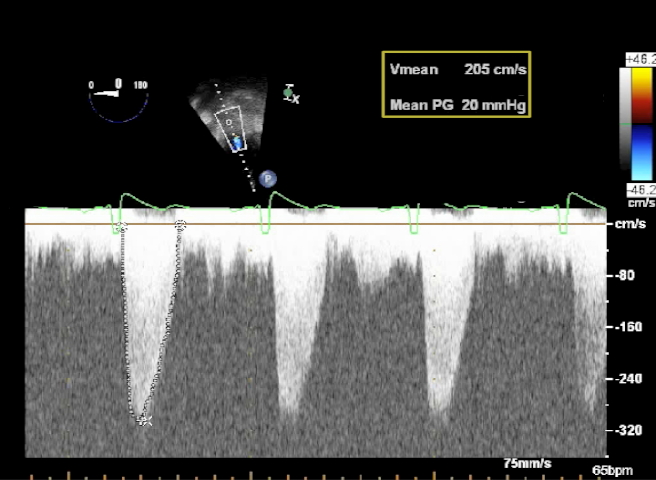
These two views are helpful in assessing the severity of aortic stenosis as they allow for alignment of the interrogating Doppler beam with the aortic outflow tract. Spectral Doppler (pulsed and continuous wave) can then be readily applied assisted by color flow. Using the modified Bernoulli Equation the peak systolic gradient across the AV can be calculated as follows:
The mean gradient is obtained by tracing the area in the spectral Doppler display corresponding to aortic flow over time
This provides a better correlation with cardiac catheterization-derived aortic gradients than estimated Doppler peak gradients. The TG LAX and DTG LAX views are also helpful in the evaluation of aortic valve regurgitation allowing the extent of the jet to be examined as it courses into the ventricle during diastole