Author: Sana Ullah, MB ChB, FRCA. Children’s Medical Center, Dallas
A 17-year-old male with a history of hypertrophic cardiomyopathy presents to cardiology clinic for routine follow-up. During transthoracic echocardiography, which of the following maneuvers is MOST likely to reveal a latent gradient across the left ventricular outflow tract?
EXPLANATION
Hypertrophic cardiomyopathy (HCM) is the most common cause of sudden death in competitive athletes. The most common etiology is ventricular arrhythmia secondary to myocardial fibrosis, microvascular coronary disease, and structural disarray of cardiomyocytes. A comprehensive evaluation for HCM includes a detailed family history as well as a thorough clinical history and physical exam with the following diagnostic work up: (1) 12-lead and Holter ECG; (2) transthoracic echocardiography (TTE) to assess wall thickness, left ventricular outflow tract (LVOT) gradient, and degree of mitral regurgitation; (3) cardiac MRI to detect late gadolinium enhancement (LGE) as a marker for fibrosis; and (4) genetic testing.
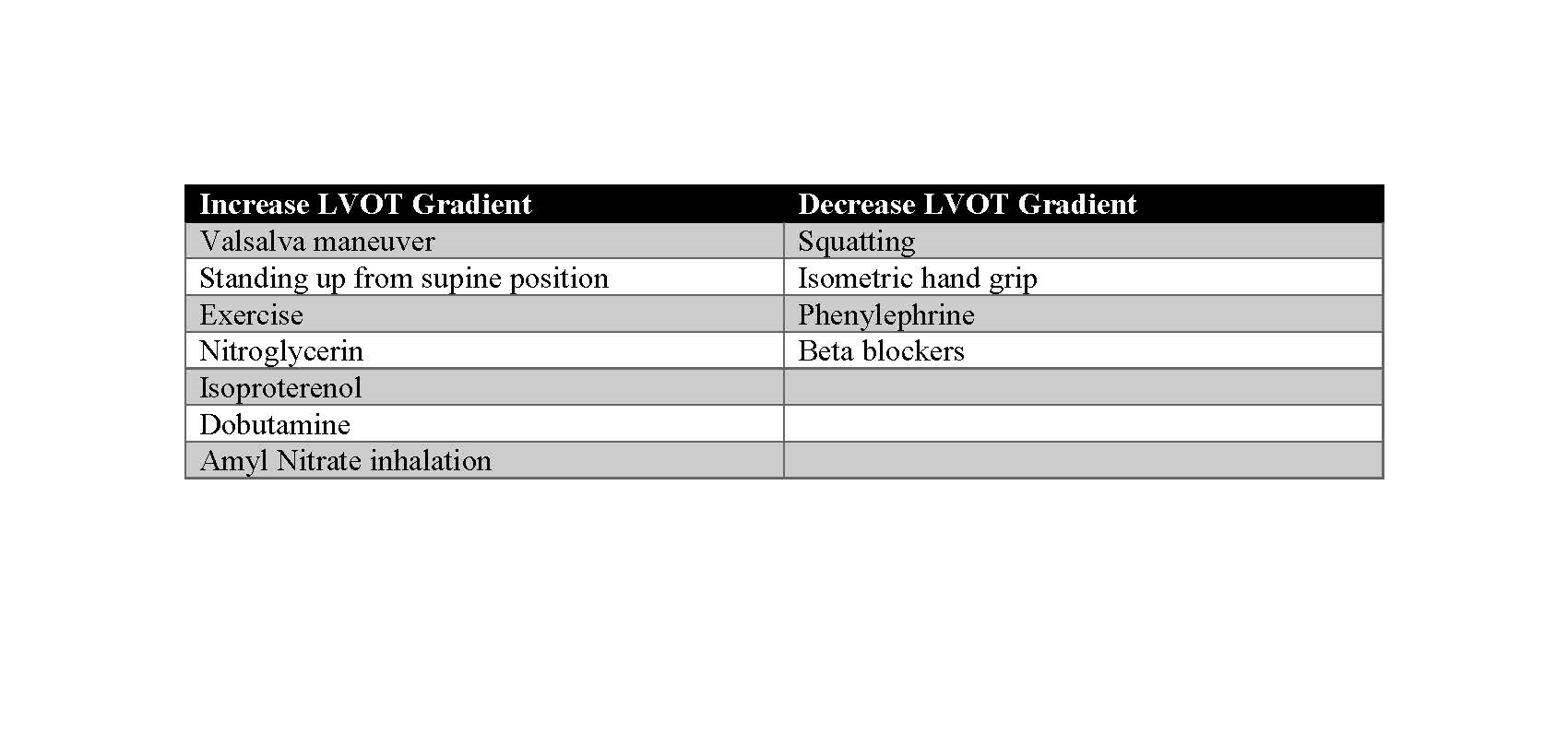
An LVOT gradient of > 50 mmHg is a hemodynamically significant gradient. If less than 50 mmHg, provocative measures may be used to assess the dynamic component of the LVOT gradient. Maneuvers that increase LV afterload, such as isometric hand grip, squatting, and phenylephrine infusion, will reduce the gradient. Factors that decrease afterload and/or increase contractility will increase the gradient and can be useful in detecting a latent gradient. TTE after stress with exercise is the preferred method to detect LVOT gradient versus pharmacologic stress. The effect of various maneuvers on the LVOT gradient are summarized in the table.
 Assessment of risk for sudden cardiac death (SCD) is a key component to managing patients with HCM. Any HCM patient surviving cardiac arrest is a candidate for secondary prevention with an implantable cardioverter-defibrillator (ICD) device. Guidelines for primary prevention have recently been published by the American Heart Association and the American College of Cardiology (1,2). Accurate risk stratification for primary prevention is important as ICDs are associated with significant morbidity. This includes inappropriate defibrillation in approximately 30% of patients as well as negative psychological repercussions and the imposition of limitations on participation in certain sports. Major factors under recommendation for risk stratification include: (1) Family history of sudden death; (2) extreme LV hypertrophy; (3) unexplained syncope; (4) non-sustained ventricular tachycardia; (5) LGE on cardiac MRI; (6) end-stage HCM, and (7) LV apical aneurysm. Family history of sudden death, extreme LV hypertrophy, and unexplained syncope are the most important factors for risk stratification of children and adolescents. Patients with one or more of these factors are candidates for an ICD device.
Assessment of risk for sudden cardiac death (SCD) is a key component to managing patients with HCM. Any HCM patient surviving cardiac arrest is a candidate for secondary prevention with an implantable cardioverter-defibrillator (ICD) device. Guidelines for primary prevention have recently been published by the American Heart Association and the American College of Cardiology (1,2). Accurate risk stratification for primary prevention is important as ICDs are associated with significant morbidity. This includes inappropriate defibrillation in approximately 30% of patients as well as negative psychological repercussions and the imposition of limitations on participation in certain sports. Major factors under recommendation for risk stratification include: (1) Family history of sudden death; (2) extreme LV hypertrophy; (3) unexplained syncope; (4) non-sustained ventricular tachycardia; (5) LGE on cardiac MRI; (6) end-stage HCM, and (7) LV apical aneurysm. Family history of sudden death, extreme LV hypertrophy, and unexplained syncope are the most important factors for risk stratification of children and adolescents. Patients with one or more of these factors are candidates for an ICD device.
REFERENCES
1. Ommen SR, Mital S, Burke MA et al. 2020 AHA/ACC guideline for the diagnosis and treatment of patients with hypertrophic cardiomyopathy. J Am Coll Cardiol . 2020;76:e159-e240. https://doi.org/10.1016/j.jacc.2020.08.045
2. Maron BJ, Desai MY, Nishimura RA et al. Management of hypertrophic cardiomyopathy: JACC State-of-the-Art Review. J Am Coll Cardiol .2022; 79:390-414. https://doi.org/10.1016/j.jacc.2021.11.021
3. Maron BJ, Desai MY, Nishimura RA et al. Diagnosis and evaluation of hypertrophic cardiomyopathy: JACC State-of-the-Art Review. J Am Coll Cardiol . 2022; 372-389. https://doi.org/10.1016/j.jacc.2021.12.002
