Author: Sana Ullah, MB, ChB, FRCA - Children’s Medical Center, Dallas
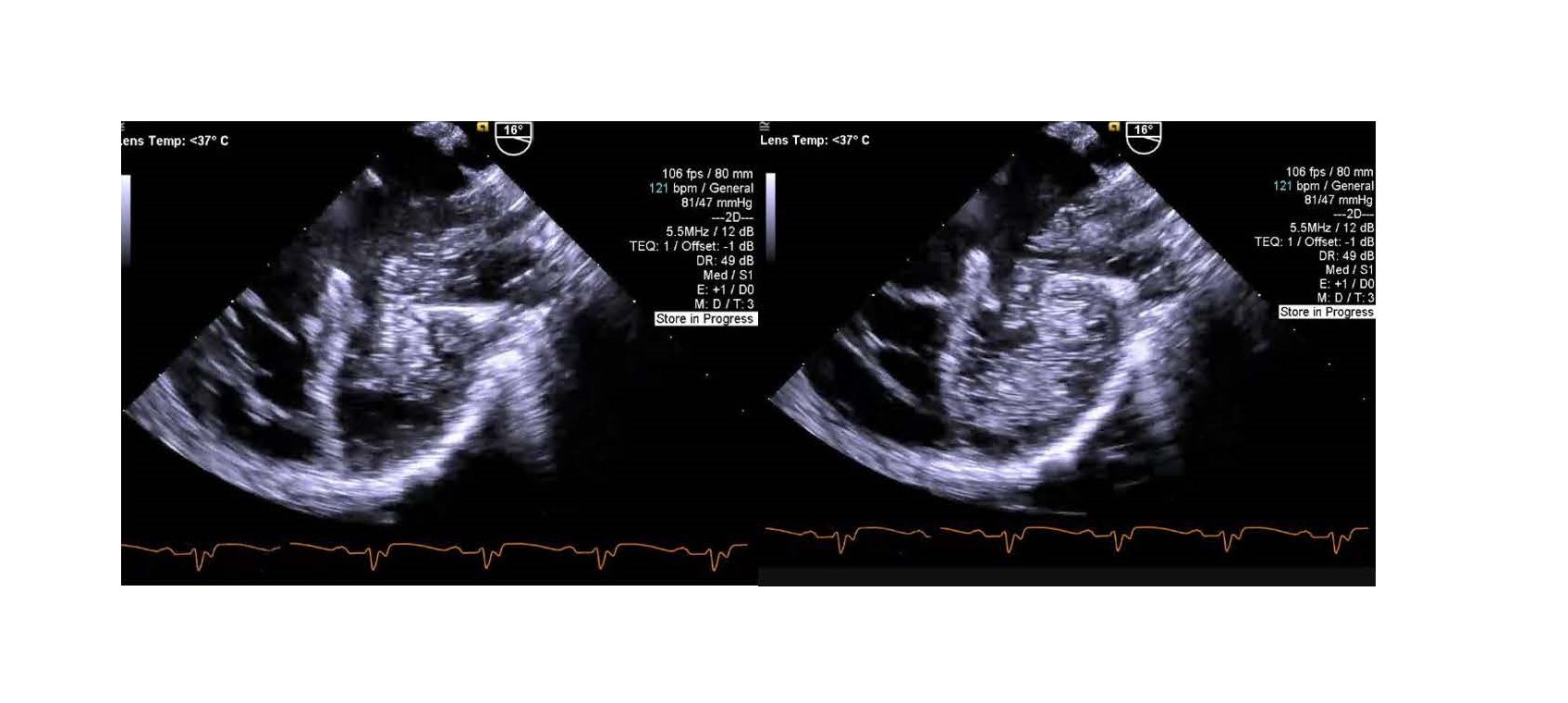
A 3-year-old female toddler with a large atrial septal defect (ASD) in addition to dysplastic mitral and tricuspid valves (both with severe regurgitation) presents for repair of both valves and ASD closure. After intubation, vital signs are as follows: HR 120, BP 90/50, SpO2 92%. During the pre-bypass transesophageal echo (TEE), agitated saline contrast is injected into a left arm peripheral IV with two of the TEE images demonstrated below. What is the MOST likely diagnosis?
EXPLANATION
In the TEE images above, contrast is clearly seen entering the left atrium initially and then into the left ventricle, confirming the presence of a left superior vena cava (LSVC) draining into an unroofed coronary sinus. A persistent LSVC is found in approximately 4% of patients with congenital heart disease compared with 0.5% in the general population. In 80-90% of cases, it drains into the right atrium via the coronary sinus. In 10-20% of cases, the LSVC drains into the left atrium due to partial or complete absence of the “roof” of the coronary sinus. It can be diagnosed with echocardiography by injecting agitated saline contrast into an IV placed in the left arm.
An unroofed coronary sinus has several important clinical implications including: (1) It is a source of right to left shunting (often called a coronary sinus ASD) leading to mild cyanosis; (2) It can lead to systemic thromboembolism, potentially resulting in an ischemic stroke or cerebral abscess; (3) It can impact repair of an ostium primum ASD and usually requires baffling into the right atrium.
A persistent LSVC also has important clinical implications: (1) It may require additional venous drainage cannulation during cardiopulmonary bypass cases, depending on the presence of a bridging vein; (2) An unrecognized LSVC can be a source of systemic desaturation in a bidirectional cavopulmonary anastomosis or a Fontan; (3) A heart transplant recipient with a LSVC will require modification to the venous drainage anastomoses; (3) It may render retrograde cardioplegia ineffective; (4) It can complicate procedures such as central venous cannulation or pacemaker implantation.
Pulmonary arteriovenous fistulas are congenital or acquired intrapulmonary right-to-left shunts. The diagnosis can be confirmed with echocardiography by showing a shortened transpulmonary transit time from the right heart to the left atrium during injection of contrast into a peripheral IV.
A sinus venosus defect will show contrast entering the right atrium first, and therefore, answer C is incorrect.
REFERENCES
1. Azizova A, Onder O, Arslan S, Ardali S, Hazirolan T. Persistent left superior vena cava: clinical importance and differential diagnoses. Insights into Imaging. 2020. 11:110. https://doi.org/10.1186/s13244-020-00906-2
2. Ootaki Y, Yamaguchi M, Yoshimura N et al. Unroofed coronary sinus syndrome: diagnosis, classification, and surgical treatment. J Thorac Cardiovasc Surg. 2003; 126:1655-6. doi:10.1067/S0022-5223(03)01019-5
