Authors: Kaitlin M. Flannery, MD, MPH - Stanford University AND Catherine Dietrich, MD - Stanford University
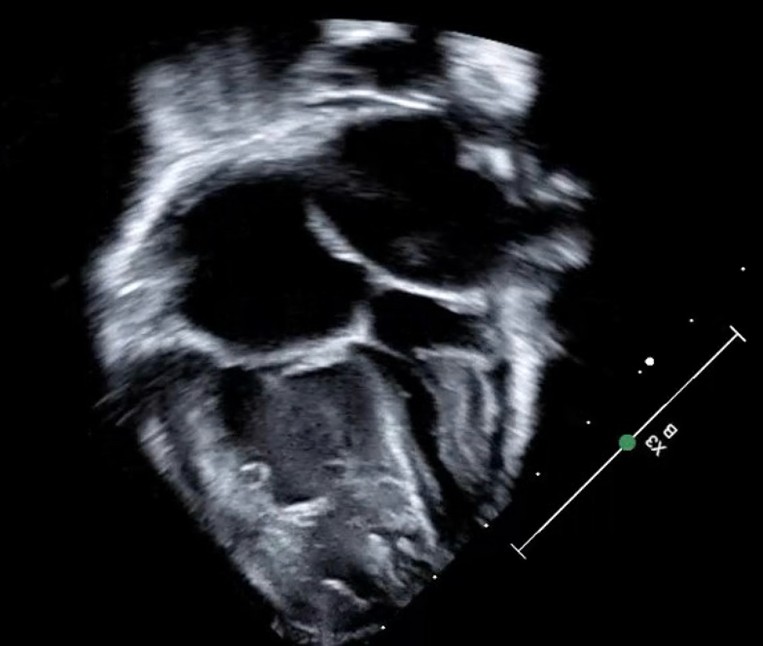
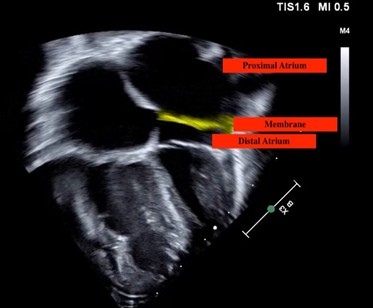
A 5kg, 4-month-old infant with feeding intolerance and failure to thrive is noted to have a murmur on pediatrician follow up visit. A 4-chamber view of his transthoracic echocardiogram is shown below. What is the MOST LIKELY diagnosis identified in this image?
EXPLANATION
Cor triatriatum (from the Latin for a “heart with three atria”) is a rare cardiac anomaly that results from abnormal septation of either the right (dexter – from the Latin for “right-sided or right-handed”) or left (sinister – from the Latin for “left-sided or left-handed”) atrium. It occurs in less than 0.1% of all congenital heart disease. In classic cor triatriatum sinister (CTS), which was present in the patient above, a fibromuscular membrane divides the proximal atrium, which accepts pulmonary venous return, from the distal atrium which contains the atrial appendage and mitral valve. The membrane may be complete, incomplete, or fenestrated. The severity of the membrane gradient, and presence or absence of other cardiac anomalies, will determine the age and status at presentation.1
CTS symptoms and management emulate that of mitral stenosis. Restriction of flow across the membrane results in elevated left atrial pressure which leads to elevated pulmonary venous pressure and pulmonary edema. The elevated pulmonary venous pressure will cause elevated pulmonary arterial pressure that can become permanent if left untreated. High left atrial pressure can result in left atrial dilation increasing risk for atrial arrhythmias and thrombus formation. If the flow gradient significantly limits left ventricular filling, a low cardiac output state may develop.1
Induction of anesthesia for surgical correction requires maintenance of preload with judicious fluid administration, maintenance of sinus rhythm and avoidance of tachycardia to allow ventricular filling, and avoidance of increases in pulmonary vascular resistance (PVR) that will put additional strain on the right ventricle. Prior to surgical removal of the membrane, therapies that decrease PVR should be limited as they might cause pulmonary congestion. After removal of the membrane, PVR-lowering therapies can be employed.1
As cor triatriatum remains a rare anomaly, there are limited large studies assessing surgical outcomes. The largest one to date is a descriptive retrospective review of 65 patients treated from 1963-2010 at Boston Children’s Hospital. The median age at surgical repair was 6.9 months with a range from 2 days to 47 years. Over half of the patients were infants. Additional cardiac anomalies were found in 75% of the patients, with atrial septal defect, ventricular septal defect, and partial anomalous pulmonary venous return being the most common. The two deaths that occurred in the early postoperative period were in infants operated on in the 1970’s. In the remaining patients, there was no recurrence of obstruction in the atrium. However, approximately 10% developed pulmonary vein stenosis that required interventional or surgical management.2
A more recent retrospective review describes 16 patients treated from 2000-2020 at the University of Minnesota. The median age at diagnosis was 4.3 months with a range from 1 day to 7 years. Additional cardiac anomalies were found in 81% of the patients. The CTS created a clinically significant obstruction in 50% of patients. Twelve patients underwent surgical repair. Two patients had early postoperative surgical mortality. These patients had additional congenital cardiac anomalies, one with heterotaxy and complex single ventricle anatomy and one with total anomalous pulmonary venous return. The remaining 10 surgical patients did well with no recurrence of obstruction in the atrium on follow-up.3
The image in the scenario clearly shows a left atrial membrane, effectively separating it in proximal and distal portions. Cor triatriatum dexter would result from a right atrium membrane, and no membrane would be seen in context of pure mitral stenosis.
REFERENCES
1. Kumar Jha A, Makhija N. Cor Triatriatum: a review. Semin Cardiothorac Vasc Anesth. 2017 Jun;21(2):178-85.
2. Kazanci SY, Emani S, McElhinney DB. Outcome after repair of cor triatriatum. Am J Cardiol. 2012 Feb 1;109(3):412-6.
3. Mashadi AH, Narasimhan SL, Said SM. Cor triatriatum sinister: long-term surgical outcomes in children and a proposal for a new classification.J Card Surg. 2022 Dec;37(12):4526-33.
