Author: Nicholas Houska, DO and Dustin Nash, MD - University of Colorado, Children’s Hospital Colorado
A 4-month-old infant has just undergone repair of Tetralogy of Fallot with a transannular patch, removal of right ventricular muscle bundles and ventricular septal defect (VSD) closure. Six hours postoperatively, the patient’s heart rate gradually increases to 230 beats per minute with concurrent hypotension. The electrocardiogram (ECG) demonstrates a narrow complex tachycardia. An atrial electrogram is performed and illustrated below (From author’s library). What is the MOST likely diagnosis?

EXPLANATION
Junctional ectopic tachycardia (JET) is an arrythmia most frequently seen in infants and children. It may be congenital in nature, but more commonly occurs postoperatively after cardiac surgery. JET originates from the area near the atrioventricular (AV) node and Bundle of His. It is most frequently associated with VSD closure, repair of Tetralogy of Fallot, and atrioventricular septal defect repair. Other risk factors for the development of JET include age less than 6 months, prolonged surgical time, prolonged cross clamp time, and the use of inotropes. The pathophysiology of postoperative JET is incompletely understood but is thought to be associated with trauma, stretch, and ischemia of the conduction system leading to the loss of cell membrane integrity. The etiology is likely multi-factorial but is ultimately related to increased sympathetic tone and automaticity. JET can be associated with significant morbidity and mortality. Additionally, it may be difficult to diagnose and treat. JET occurs with a frequency of 5-10% after congenital cardiac surgery. For these reasons, it is important for clinicians to have a high index of suspicion for JET and provide prompt diagnosis and treatment.
Junctional ectopic tachycardia is typically a narrow complex tachycardia with ventriculo-atrial (VA) dissociation. The ventricular rate is typically irregular and higher than the atrial rate except in the less common instance of one to one (1:1) VA conduction. Onset is gradual with no initiating ectopic beat. Patients with JET have a heart rate greater than the 95th percentile for age, otherwise it is termed accelerated junctional rhythm. Diagnosis can be difficult on a standard surface ECG due to the difficulty in identifying atrial depolarization (P wave). In patients with atrial pacing leads, an atrial electrogram can be performed by connecting the atrial lead directly to one of the leads on a standard ECG. This allows identification of atrial depolarization in side by side comparison with ventricular depolarization in the other leads. The ECG below shows dissociation of ventricular depolarization (V) at a rate of 195 beats per minute (bpm) from atrial depolarization (A) at a rate of 170 bpm, which confirms the diagnosis of JET. Red squares are highlighting the association of QRS complexes on the standard ECG with the signals on the atrial electrogram.
Postoperative JET is typically self-limited, but treatment may be indicated for hemodynamic instability. Treatment includes attenuating sympathetic stimulation by reducing inotrope dose, optimizing analgesia and sedation, and administration of dexmedetomidine. Correction of electrolytes and induction of mild hypothermia are also mainstays of treatment. Adenosine will not terminate JET but will cause AV dissociation when JET is difficult to identify. Amiodarone is the drug of choice for treatment. In refractory cases with hemodynamic instability, extracorporeal membrane oxygenation and/or catheter ablation may be indicated.
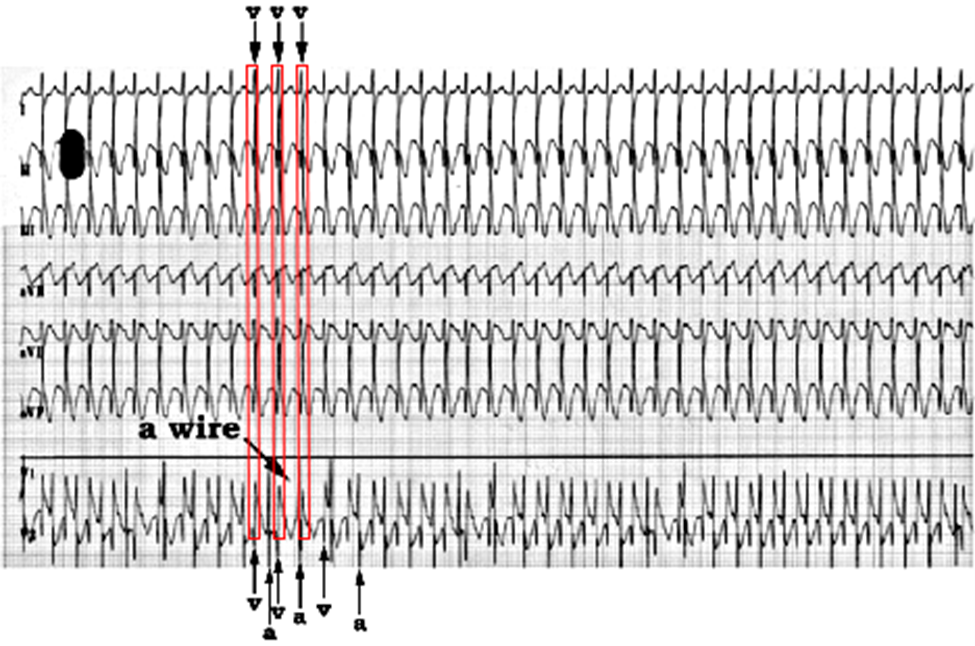 (Source: author’s library)
(Source: author’s library)
REFERENCES
Alasti M, Mirzaee S, Machado C, et al. Junctional ectopic tachycardia (Jet). J Arrhythmia .2020;36(5):837-844.
Kaltman JR, Madan N, Vetter VL, Rhodes LA. Arrhythmias and sudden cardiac death. In: Pediatric Cardiology. Elsevier; 2006:171-194.
Sasikumar N, Kumar R, Balaji S. Diagnosis and management of junctional ectopic tachycardia in children. Ann Pediatr Card. 2021;14(3):372.
Ashraf M, Goyal A. Junctional ectopic tachycardia. In: StatPearls. StatPearls Publishing; 2023. Accessed July 21, 2023. https://www.ncbi.nlm.nih.gov/books/NBK560851/
