Author: Meera Gangadharan, MD, FASA, FAAP - University of Texas at Houston
A neonate presents with cyanosis, tachypnea, and poor oral intake. Vital signs are HR 180, BP 60/40, RR 64, SpO2 75% in room air. A transthoracic echocardiogram demonstrates severe right atrial enlargement, severely depressed right ventricular function with moderate tricuspid regurgitation and leaflets in the normal location, and a severely thinned right ventricular free wall with bidirectional shunting across a patent foramen ovale. Left heart structures are normal. An electrocardiogram shows sinus tachycardia. What is the MOST likely diagnosis?
EXPLANATION
This newborn has a rare cardiac condition called Uhl’s anomaly, which is characterized by a very dilated, and poorly functioning right ventricle (RV). The free wall of the RV is dilated and paper-thin due to the absence of a myocardial muscle layer except for the cardiac apex where muscular trabeculations may be present. The pathogenesis is still debated but abnormal apoptosis of the RV myocardium is the most likely explanation as the myocardium is evident in early gestation. Biopsies are also notable for the absence of myocardial inflammation.
Fetal diagnosis can be challenging but has important implications for prognosis as Uhl’s anomaly differs from other diagnoses that are similar. The papillary muscle of the tricuspid valve can be mistaken for the septal leaflet of the tricuspid valve, making it appear to be apically displaced. Magnetic resonance imaging (MRI) will typically demonstrate a pathognomonic absence of the myocardial muscle layer between the RV epicardium and endocardium. This is demonstrated in the illustration below. Patients usually present in the newborn period or infancy with signs of right heart failure, although there are case reports of adults with this condition. There may be tricuspid and pulmonary valve abnormalities as well. Left heart structures and the coronary arteries are typically normal.
Treatment includes medical management with diuretics, digoxin, and beta blockers. Surgical options are generally determined by the specific anatomical substrate, but generally involve RV-exclusion procedures such as the Glenn, Fontan or one-and-a-half ventricle repairs which may include plication of excess right ventricular free wall. Cardiac transplantation may also be a treatment modality.
The two main diagnoses on the differential with Uhl’s anomaly are arrhythmogenic right ventricular cardiomyopathy (ARVC, previously called arrhythmogenic right ventricular dysplasia) and Ebstein’s anomaly. ARVC is characterized by arrhythmias and sudden cardiac death, usually in late childhood or young adulthood. Characteristic MRI appearances of ARVC are the presence of patches of fibrofatty infiltration between the layers of endocardium and epicardium. The left ventricle may also be involved in arrhythmogenic cardiomyopathy. Ebstein’s anomaly is characterized by the apical displacement of the septal leaflet of the tricuspid valve with the sail-like appearance of the anterior leaflet. In contrast, the tricuspid valve leaflets insert at the true annulus of the tricuspid valve in Uhl’s anomaly. The image below is an illustration of the typical cardiac magnetic resonance imaging in Uhl’s anomaly.
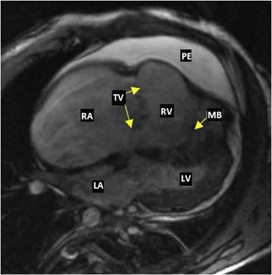
Cardiac magnetic resonance, in steady-state free precession, four-chamber sequence showing marked right chamber dilatation. The tricuspid valve (TV) has normal positioning. A moderator band (MB) and a medium-volume pericardial effusion (PE) are visualized. LA, Left atrium; LV, left ventricle;RA, right atrium;RV, right ventricle. From Faria et al. https://doi.org/10.1016/j.case.2020.05.014. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
REFERENCES
Gerlis LM, Schmidt-Ott SC, Ho SY, Anderson RH. Dysplastic conditions of the right ventricular myocardium: Uhl's anomaly vs arrhythmogenic right ventricular dysplasia. Br Heart J. 1993;69(2):142-150. doi:10.1136/hrt.69.2.142
Mihos CG, Larrauri-Reyes M, Yucel E, Santana O. Clinical presentation, and echocardiographic characteristics of Uhl's anomaly.Echocardiography. 2017;34(2):299-302
Faria B, von Hafe P, Ferreira FC, et al. Uhl's Anomaly: 10 Years of Follow-Up of an Unoperated Patient. CASE (Phila). 2020;4(5):351-355. Published 2020 Jun 24. doi:10.1016/j.case.2020.05.014
Kalita JP, Dutta N, Awasthy N, et al. Surgical Options for Uhl's Anomaly.World J Pediatr Congenit Heart Surg. 2017;8(4):470-474. doi:10.1177/2150135117710940
Vaujois L, van Doesburg N, Raboisson MJ. Uhl's anomaly: a difficult prenatal diagnosis. Cardiol Young. 2015;25(3):580-583. doi:10.1017/S1047951114000651
Corrado D, Zorzi A, Cipriani A, et al. Evolving Diagnostic Criteria for Arrhythmogenic Cardiomyopathy. J Am Heart Assoc. 2021;10(18): e021987.
