Authors: Sonya V. Gupta, AM, MS1 - Stanford University AND Kaitlin M. Flannery, MD, MPH - Stanford University
A 2-year-old, 10kg female with DiGeorge syndrome, reactive airway disease, and history of Tetralogy of Fallot with pulmonary atresia and major aortopulmonary collaterals (MAPCAS), who has undergone unifocalization and complete intracardiac repair with RV-PA conduit, presents to the cardiac catheterization lab for conduit and pulmonary artery dilation. The procedure is complicated by pulmonary hemorrhage, requiring urgent intervention and ICU admission. According to PREDIC3T (Procedural Risk in Congenital Cardiac Catheterization), which of the following factors MOST increased the risk of the high-severity adverse event (HSAE) that occurred?
EXPLANATION
Catheterization laboratory-based procedures have expanded considerably in recent years, as has the complexity of patients and interventions. To update catheterization lab risk stratification with some of these novel procedures, the PREDIC3T (Procedural Risk in Congenital Cardiac Catheterization) study was published in 2022. The risk stratification system was created looking at the incidence of adverse events in over 23,000 catheterizations at 13 different institutions from January 2014 - December 2017. Importantly, this period included transcatheter pulmonary valve replacement (TPVR), which is missing from older risk stratification systems
Adverse events were categorized as level 1-5, with 3-5 being high-severity adverse events (HSAE). Level 1 was a near-miss, such as an equipment malfunction with no consequence. Level 2 was a minor event that was not life-threatening, such as a groin hematoma or a self-resolving hemodynamically stable arrhythmia. Level 3 was a moderate event, which could be life-threatening if not treated, such as an unstable arrhythmia or vascular injury that requires treatment. Level 4 is a major event that is life-threatening and requires CPR, surgical treatment, major interventional procedure, or ECMO to treat. Level 5 is a catastrophic event resulting in death. Adverse events occurred in 10.9% of cases, including HSAEs in 5.2% of cases. A total of 17 deaths occurred for a rate of 0.07%.1 Of note, case complexity is also increased if multiple procedures are being performed together.1-2
The following patient factors were found to be significantly associated with HSAEs1:
● Age < 30 days
● Single ventricle physiology
● Cardiac surgery in the past 90 days
● Low systemic oxygen saturation (<95% for biventricular physiology, <78% for single ventricle)
● Low mixed venous saturation (<60% for biventricular physiology, <50% for single ventricle)
● High pulmonary artery pressure (PASP > 45 mmHg for biventricular physiology, mPAP > 17 mmHg for single ventricle)
● Systemic ventricle end-diastolic pressure ≥18 mmHg
● Qp:Qs > 1.5:1
● PVR > 3 iWU
The following patient factors were not found to be significantly associated with HSAEs1:
● Genetic syndromes
● Noncardiac problems (ex: chronic lung disease, coagulation disorder)
The case types were divided into six risk categories (Table 1). The frequency of HSAE in risk category 0 was 1.1% and 7.7%, 10.8%, and 13.9% for categories 3, 4, and 5, respectively.1
Table 1. PREDIC3T Case-Type Risk Categories
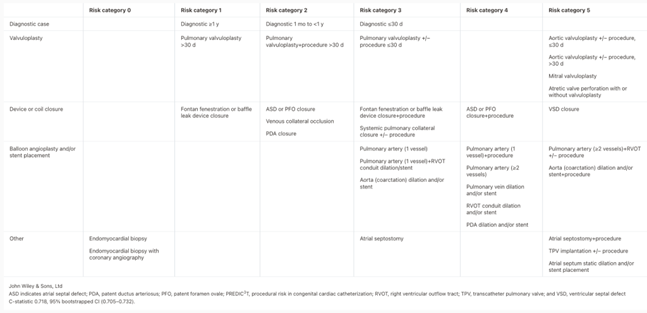 Table from: Quinn BP, Yeh M, Gauvreau K, et al. Procedural Risk in Congenital Cardiac Catheterization (PREDIC3T). J Am Heart Assoc. 2022;11(1):e022832. Used under Creative Commons License.
Table from: Quinn BP, Yeh M, Gauvreau K, et al. Procedural Risk in Congenital Cardiac Catheterization (PREDIC3T). J Am Heart Assoc. 2022;11(1):e022832. Used under Creative Commons License.
The patient in the question stem is presenting for a case that falls in risk category 5 due to intervention on ≥ 2 pulmonary arteries and RV-PA conduit intervention. The other answer choices, her genetic syndrome and noncardiac condition, are not associated with increased risk of HSAE in the PREDIC3T study.
REFERENCES
1. Quinn BP, Yeh M, Gauvreau K, et al. Procedural Risk in Congenital Cardiac Catheterization (PREDIC3T). J Am Heart Assoc. 2022;11(1):e022832. doi:10.1161/JAHA.121.022832
2. Kobayashi D, Amin EK, Morgan GJ, et al. Usefulness of PREDIC3T Case Type Risk Category in the CRISP Registry. Am J Cardiol. 2024;212:73-79. doi:10.1016/j.amjcard.2023.11.056
