Denise Joffe, MD
Associate Professor of Anesthesiology
Attending Anesthesiologist
Seattle Children’s Hospital and
The University of Washington Medical Center
Seattle, Washington
Aarti Bhat, MD
Assistant Professor of Pediatric Cardiology
Seattle Children’s Hospital
Atrial septal defects (ASD) constitute 7-10 % of all congenital heart disease. Secundum defects are the most common subtype (60-75%), followed by primum defects (20%), sinus venosus defects (SVASD) (10%), and coronary sinus defects (CS ASD). The following description is relevant to all subtypes of defects but there are special additional considerations with primum ASDs described below.
Brief clinical description:
- Clinical features of ASDs depend on the size and location of the defect as well as the age and associated lesions of the patient. As the pulmonary vascular resistance (PVR) falls and right ventricular (RV) compliance increases after birth, there is increased shunting from the left atrium (LA) to the right atrium (RA) across the defect. Over time, there is dilatation of right sided structures because of the greater volume of blood, resulting in symptoms of pulmonary overcirculation. Patients with ASDs may present as adults with unrepaired disease since only about 5% develop Eisenmenger’s syndrome if untreated.
- Device closure is often an option for patients with a secundum ASD. All other ASDs require surgical closure.
- Transthoracic echocardiography (TTE) is the mainstay of this diagnosis. On occasion, additional imaging modalities (CT, MRI and rarely TEE) may be required, more typically in situations with abnormal pulmonary venous drainage or unusual septal anatomy.
- Intraoperative TEE is used to confirm the preoperative diagnosis and verify the adequacy of repair.
Key echocardiographic evaluation pertinent to all ASDs:
- Right heart enlargement (RA, RV and pulmonary artery (PA)): Qualitative grading of RV dilation compares the RV apex to the LV apex (mild enlargement- RV/LV=⅔, mod enlargement- RV=LV, Severe enlargement – RV>LV).
- Associated lesions in “isolated ASDs”: Left superior vena cava (LSVC), mitral regurgitation (MR), pulmonary valve stenosis (PS), and partial anomalous pulmonary venous drainage (PAPVD).
- Significant moderate or severe tricuspid regurgitation (TR) may occasionally result from right ventricular enlargement (RVE) or pulmonary hypertension (PHTN) and is more common in older patients. It is crucial to verify that irreversible PHTN does not exist prior to closing an ASD. Evaluation of RV systolic pressure (as an estimate of pulmonary artery systolic pressure (PASP) is done qualitatively by looking for right ventricular hypertrophy (RVH), the position of the interatrial and interventricular septum (IAS, IVS) and the direction of atrial shunting. A leftward interatrial and interventricular septal position in systole and bidirectional or right to left shunting is suggestive of PHTN. More quantitative estimates of pulmonary artery pressure use the peak gradient of the TR jet to estimate PASP, and the end diastolic velocity of the pulmonary insufficiency (PI) jet to estimate pulmonary artery diastolic pressure (PADP). However, it is crucial to understand that in the event of concern for significant PHTN, the patient requires a cardiac catheterization to measure PVR since PAP alone is not a measure of the ability to tolerate ASD closure.
- Evaluation of the atrial septum in multiple orthogonal views is essential to assess the size, the number of defects, their rims and relation with other structures such as the superior and inferior vena cava (SVC and IVC), coronary sinus ostium, tricuspid valve, and right sided upper pulmonary vein (RUPV).
- Biventricular systolic function assessment.
TTE imaging
An ASD is a three-dimensional structure even though it is described in serial uniplanar views. With TTE, the superior and inferior rims of secundum ASDs are best determined in the apical four chamber and subcostal coronal views. The anterior retroaortic and postero-inferior rims are best determined on the parasternal short axis. The subcostal short axis view demonstrates the antero-superior rim of the atrial septal defect and its proximity to the SVC-RA junction. The septal length, defect and rim dimensions can be measured in each of these views for review with interventional cardiology colleagues with regard to device sizing and feasibility of deployment to a safe position without complications.
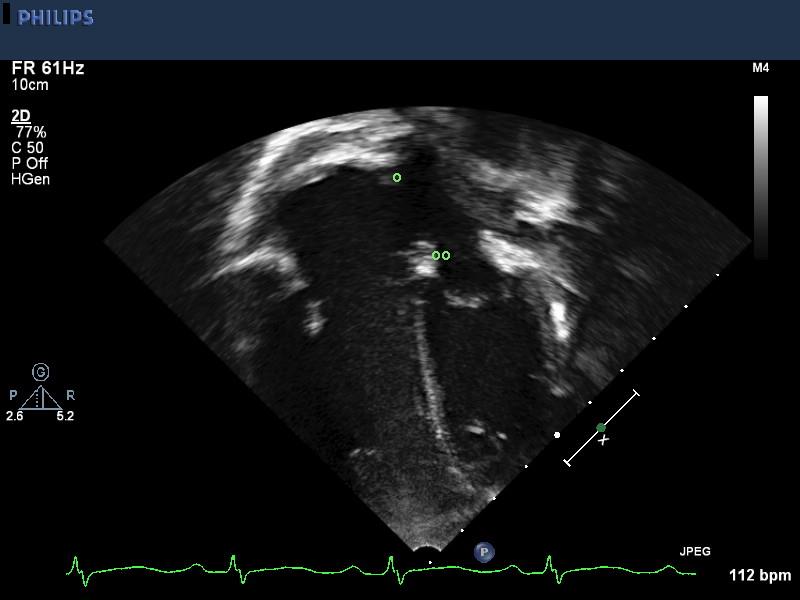
Apical four-chamber view shows the relative proportion of the right and left sides of the heart. There is right atrial as well as right ventricular dilatation. The superior-inferior anatomy of the ASD is well seen including a T sign to the superior (o) as well as inferior (oo) rims.
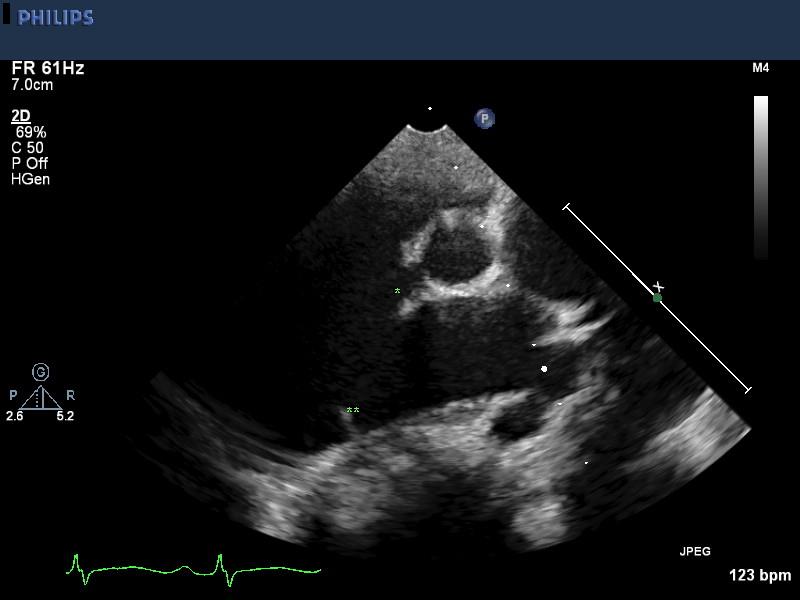
High parasternal views shows PA anatomy. There is significant PA dilation (edges marked with white asterisks). There may be some increase in peak velocity across the pulmonary valve due to the overall increase in transpulmonary flow. Pulmonary valve stenosis secondary to dysplasia must be excluded.
Parasternal short axis views (PSAX) show the antero-posterior anatomy of the interatrial membrane. The anterior retroaortic (*) as well as posterior rims (**) are clearly seen. The left atrium is of normal size while the right atrium is significantly dilated.
Subcostal sagittal or short axis view demonstrates the antero-superior rim of the ASD (^) as well as its relation to the SVC, SVC-RA junction. This bicaval view is very useful in demonstration of sinus venosus defects. A superior sinus venosus defect would be seen as a defect in the region marked ^ and accompanied by partial anomalous venous drainage of the right upper pulmonary vein to the top of the defect. An inferior sinus venosus defect would appear as a deficiency in the interatrial membrane just above the insertion of the inferior vena cava into the right atrium.
Parasternal long axis view (PLAX) shows right ventricular dilatation. An atrial septal defect is typically not well seen in this view, even with inferior angulation of the probe. However, a complete and segmental study is a pre-requisite for a complete and accurate study and should be undertaken at the outset of evaluation for an atrial septal defect
Parasternal short axis (PSAX) shows dilatation of the right ventricle. Volume overload of the right ventricle causes flattening of the interventricular septum in diastole. Pressure overload of the right ventricle causes flattening of the interventricular septum in systole. This can be better appreciated on an M mode analysis of this plane.
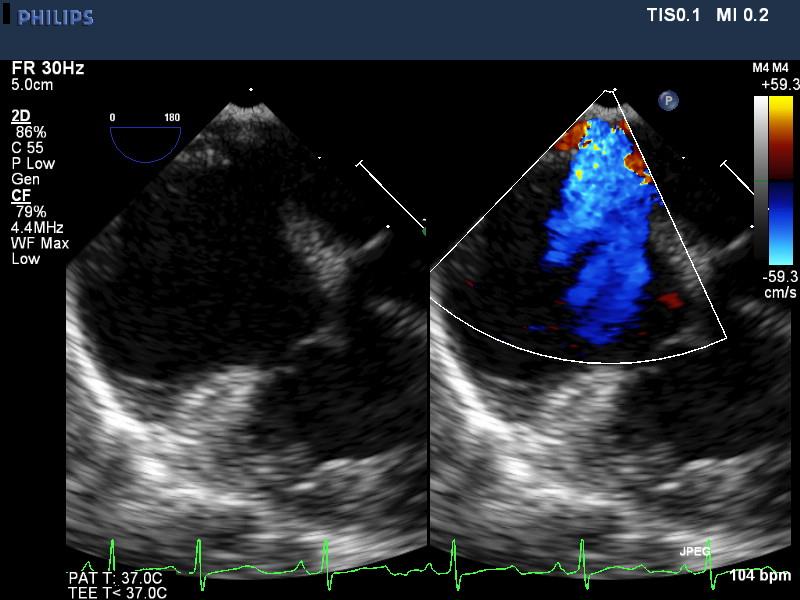
Color compare color Doppler image of the atrial septal defect in parasternal short axis views shows a wide swath of color crossing from the left atrium to the dilated right atrium indicating a large atrial septal defect. Defect measurements should be made on 2D and not color images as there is ‘bleeding’ of color into surrounding tissues and resulting over-estimation of defect sizes. In this same view, the drainage of all pulmonary veins can be determined on color Doppler as well as spectral Doppler.
Subcostal long axis sweep shows the relative location of the atrial, systemic venous and pulmonary venous structures.
Color compare apical 4 chamber view demonstrating a sinus venosus and secundum ASD. Also, there is significant right sided atrial and ventricular dilatation.
Subcostal short axis color compare view showing a superior sinus venosus ASD.
Three dimensional image from trans-esophageal imaging shows a large centrally located with deficient posterior rims as seen from the right atrium. There are no additional defects. The tricuspid valve is seen in the right lower part of the screen image and the SVC is above. 3D imaging can reveal multiple nuances of septal anatomy as well as spatial relationship to other structures and can help procedural planning for device closure of ASDs.
TEE imaging
See addendum 1 for best imaging views of ASDs
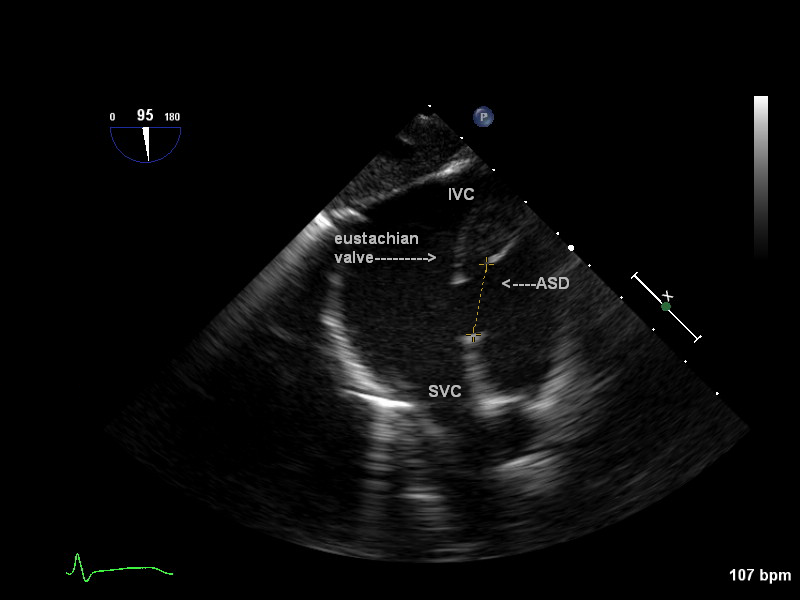
A secundum ASD is present in the area of the Fossa Ovalis. The entire septum should be examined as the probe is withdrawn until the SCV is seen entering the RA and then advanced until the IVC is seen entering the RA.
demonstrating a large secundum ASD (crosses). This retroaortic view shows the anterior-posterior dimensions of the defect. Note there is minimal retroaortic rim in this patient.
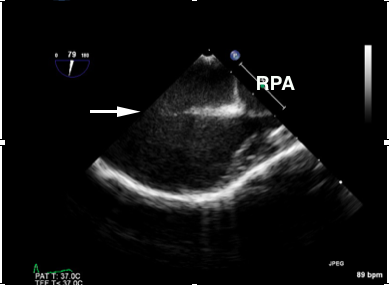
demonstrating a large secundum ASD (white arrow). This view provides the superior-inferior (longitudinal dimensions) of the defect. Note the entirety of the defect is not seen in this image. Also, there is significant enlargement of the RPA
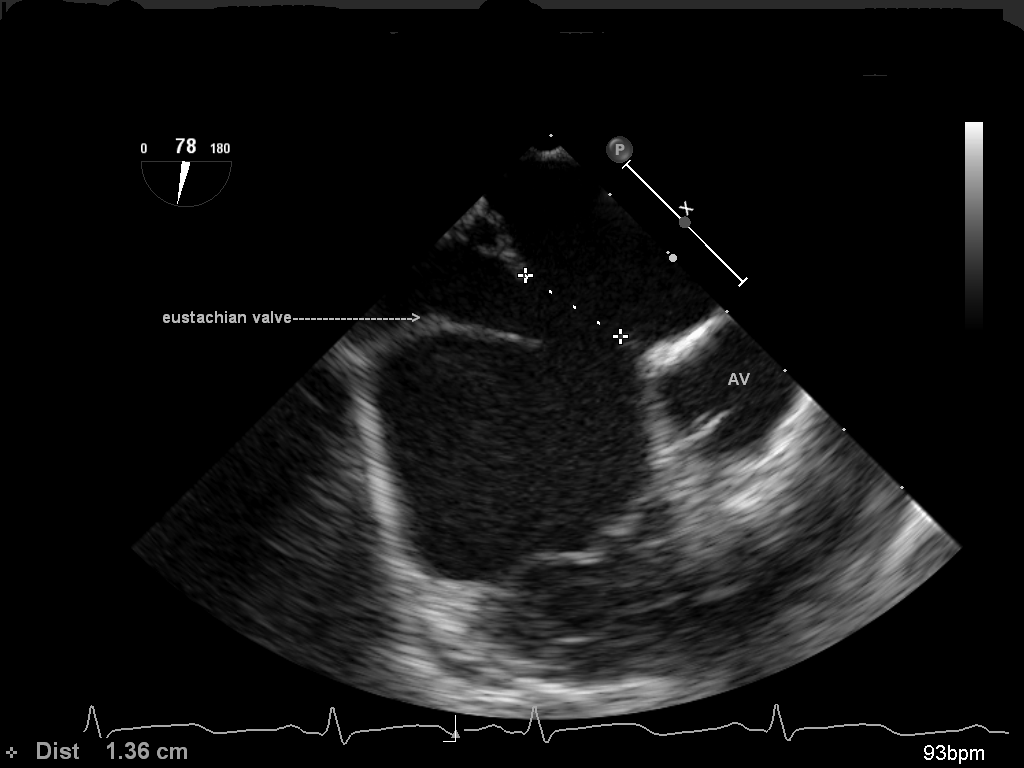
Deep transgastric bicaval view demonstrating a secundum ASD. This view also provides the superior-inferior or longitudinal dimensions of the defect. It is obtained by advancing the probe deep into the stomach, placing the RV in the field and rotating to 90 degrees. Pulling up and turning the probe to the right will display the cavae. Do not confuse the eustachian valve for the inferior portion of the defect.
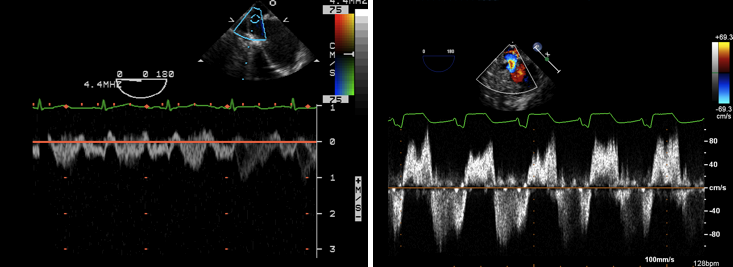
PW Doppler of the flow across an ASD. In a, the flow is predominantly left to right with a brief reversal of flow at the start of systole. In b there is bidirectional flow across the ASD which is suspicious for elevated RV pressures (pulmonary hypertension) since flow is left to right in diastole but right to left during systole.
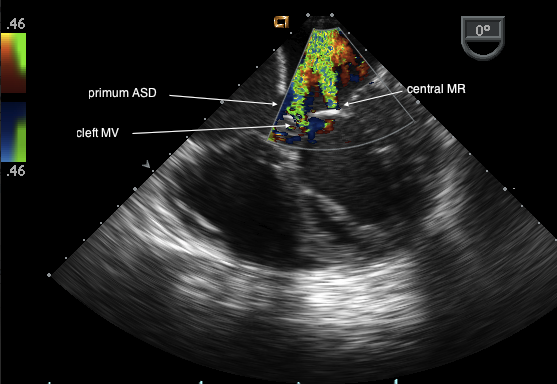
Note the primum defect in the inferior part of the interatrial septum. The AVV are at the same level consistent with an endocardial cushion defect. There are two jets of MR the most medial is through a cleft in the anterior leaflet of the mitral valve.
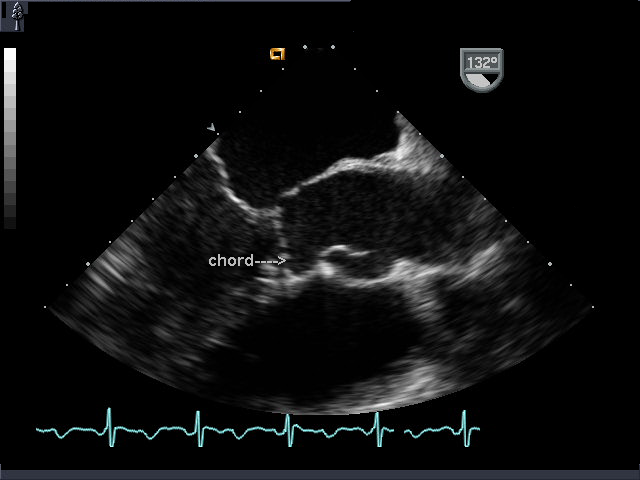
ME AV LAX view in a patient with a partial AV canal and a chord from the mitral valve that inserts into the interventricular septum. Although the chord crossed the LVOT, there was no LVOTO.
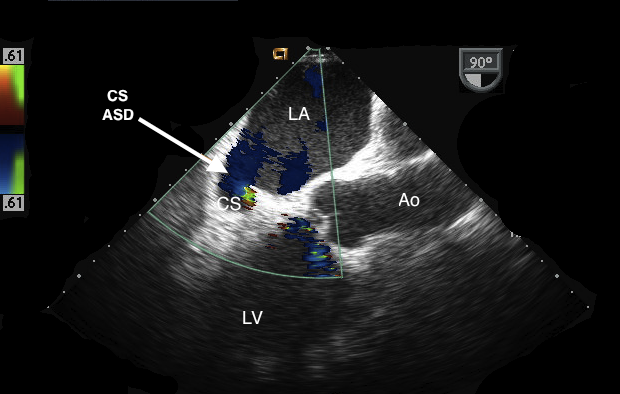
ME AV LAX view with the CS opening into the LA. Flow is left to right from the LA through the CS into the RA. Note that this patient did not have an LSVC which is consistent with the enlarged but not massive CS.
ME 4 chamber view demonstrating a patch dehiscence of a secundum ASD.
TG basal short axis view. This video shows a cleft in the anterior leaflet of the mitral valve in a patient with a partial AV canal.
ME LAX view in a patient years after repair of a partial AV canal. There is severe tunnel like LVOTO secondary to a “gooseneck deformity”. The aortic valve is well above the LVOTO and is almost out of the image. The patient also has severe MR with PISA forming at a velocity of 122 cm/sec.
ME 4 C view with probe turned to the right. Starting at the entrance of the SVC to the RA, it is then advanced almost to the entrance of the IVC into the RA. Note that at the most superior part of the IAS is a superior sinus venosus ASD. No anomalous PV are seen in this 2D image.
ME 4 C view with the probe turned to the right and withdrawn almost to the level of the SVC. A defect is seen in the superior part of the IAS with left to right flow (blue jet). Also seen is a PV (red jet) entering the right atrium.
ME bicaval view. Post repair of SVASD with PAPVD. Note the baffle directing PV flow into the LA. The SVC flow must be carefully examined to ensure that there is no obstruction to inflow by the baffle. On this view the SVC appears narrow but the flow is laminar.
A-Secundum atrial septal defects:
Key anatomical points:
- The defect includes the area of the fossa ovalis. Size: small (<6mm), moderate (6-12mm) or large ( >12mm) (in adults). Quantifying defect size in children is more variable as it depends on its size relative to the age and size of the child.
- There may be multiple defects.
Surgical/interventional management:
- The defect is closed with a device in the catheterization laboratory or in the operating room with a pericardial patch or a simple stitch closure if the defect is small although it is rare to require surgery for a small defect unless it is part of a more complex CHD.
- Criteria for device closure: In adults; defect is less than 35 mm and there is more than 5 mm of rim on all sides, i.e. between it and the aorta anteriorly, the orifices of the cava (superiorly and inferiorly), and the coronary sinus and atrioventricular valves inferiorly and the right sided pulmonary veins. More than one device may be needed for multiple defects. In children, device candidacy is decided by a number of factors including the size of the defect and its rims as they compare to the overall size of the child, and available device and sheath sizes. The patient weight usually needs to be greater than 10kg due to the size of the sheath in the femoral vessel.
B- Primum ASD (aka partial AV canal, atrioventricular or endocardial cushion defect)
Key anatomical points:
- This ASD is in the postero- inferior part of the IAS in the area of the crux of the heart.
- The normal offset of the atrioventricular valves (AVV) is absent and both valves appear at the same level on a four chamber view.
- A cleft MV is almost always present with/without regurgitation. The cleft is located in the anterior leaflet of the mitral valve. A double orifice mitral valve is a rare associated abnormality.
- Secondary changes to the MV from prolonged MR can result in annular dilation and thickened leaflets with restricted motion complicating the repair. This is more common in older patients.
- Left ventricular outflow tract obstruction (LVOTO) can develop (usually years after a primary repair). The mechanisms include: 1) Deficient LV inlet compared to LV outlet causing long tunnel-like LVOTO (“gooseneck deformity”); 2) Discrete subvalvular membrane; 3) Aberrant chords inserting into the interventricular septum (IVS).
Surgical management:
- Surgical patch closure of the primum ASD.
- The cleft is stitch closed and there is often a compromise between decreasing MR and causing mitral stenosis (MS). The cleft is often closed even if there is no MR since MR can develop over time if the cleft is left open.
- If the MR is more complex or in cases of re-operation, the repair may involve annular reduction, commissurotomy, or patch augmentation of deficient leaflet tissue. If the valve cannot be repaired, a mitral valve replacement may be needed in the older patient.
- LVOTO is repaired depending on the mechanism (see above) but rarely may require a complex procedure such as a modified Konno or full Konno procedure if the aortic valve is also severely diseased.
C- Sinus venosus ASD (SVASD):
Key anatomical points:
- Absence of the common wall between the pulmonary veins (PV), RA and SVC creates an ASD and enables the PVs to drain into the RA as they course posterior to the RA on their path to the LA.
- The most common type is a superior SVASD with anomalous right upper pulmonary venous (RUPV) drainage into the RA/SVC.
- Inferior defects are very rare. Typically they involve anomalous drainage of the right lower PVs into the RA.
Surgical management:
- Patch closure of the defect with the anomalous PV baffled to the LA.
- The SVC-RA junction may be augmented with pericardial patch to avoid SVC obstruction: 2 patch technique- one to baffle the PV and one to augment the SVC.
- A Warden procedure may be necessary when the PV drains into the high SVC or if there is difficulty making an unobstructed baffle. The SVC is disconnected and reattached to the RA appendage. The PV “stump” (cardiac end of the SVC containing the anomalous PV) is baffled to the LA.
D- Coronary sinus atrial septal defects (aka unroofed coronary sinus):
Key anatomical points:
- Commonly associated with an LSVC.
- Absence of part or all of the common wall between the CS and LA as the CS courses behind the LA essentially creates an ASD with predominantly L to R shunting although some of these patients (especially with an LSVC and high volume flow) have bidirectional shunts and may be cyanotic.
- The CS may appear large even without an LSVC because of flow from the L to R shunt but it is typically extremely enlarged in the presence of an unroofed CS and LSVC. It is absolutely crucial to identify the presence of an LSVC since it alters the surgical repair.
Surgical management:
- WITHOUT AN LSVC – Simple patch closure of the CS orifice. The CS drains into the LA resulting in minimal cyanosis (small R to L shunt).
- WITH AN LSVC and bridging vein (innominate vein). Simple patch closure of CS orifice and ligation of LSVC to CS connection.
- WITH AN LSVC and no bridging vein- The roof of the CS is covered (baffled) and allowed to drain into the RA. If an LSVC is not recognized simple patch closure of the CS ostium will result in unacceptable cyanosis.
Basic echo principles when imaging patients with an ASD
What to look for on 2D:
- Classify ASD.
- Measure ASD size/area.
- Examine MV structure and function. Look for prolapse/cleft. Measure annulus.
- Examine TV structure and function. Look for prolapse. Measure annulus.
- Examine PV drainage especially right sided PVs.
- Assess for RAE, RVE qualitatively (see above).
- Assess biventricular function.
- Examine morphology/function of pulmonary valve. Look for doming leaflets, commissural fusion, and restricted motion. Measure PA size.
- Evaluate for evidence of PHTN (see above).
- Look for an LSVC draining into the CS, located between the LUPV and LAA. In a patient with an unroofed coronary sinus, a bubble study with agitated saline injected into a left hand intravenous line would opacify the LA before bubbles are seen entering the RA. If the above patient also has a bridging vein (innominate vein) opacification of the RA and LA may occur almost simultaneously. In a patient with any other ASD (except an unroofed CS ASD), opacification of both the RA and LA will occur because of the atrial communication, but opacification of the RA will precede the LA.
What to look for with Doppler:
- Color Flow Doppler (CFD) and Pulse Wave Doppler (PW) for direction of flow through ASD. (Predominant L to R in an uncomplicated ASD’s).
- CFD/PW to locate PV flow. Note that PW of PVs may show higher baseline velocities secondary to high pulmonary blood flow but pulsatility is preserved and peak and mean velocities are not significantly elevated.
- CFD/CW to grade MR, TR.
- Estimate PASP if TR is present. RVP = PASP = 4VTR2 + RAP. (Ensure no PS)
- Estimate PADP with velocity of PI end diastolic jet PADP = 4V 2 PI diastole + RAP
- CFD/CW to assess for pulmonary valve stenosis. Velocities up to 2.5 m/sec may result from ASD flow alone.
- CFD used to localize an LSVC.
Key intraoperative echocardiography points following ASD repair:
- Verify ASD closure. Bubble contrast study is often a helpful adjunct to visualize residual shunts.
- If a device closure is used, confirm device is stable without significant movement and not obstructing or impinging on PV, aorta, cavae, coronary sinus or atrioventricular valves.
- Assess MV function. After a primum repair, MR can be eccentric and composed of multiple jets. Grading can be difficult. Less than mild MR is optimal for a durable repair but more significant MR is often accepted in children to avoid early MVR. Use vena contracta width, density of spectral jet, duration of regurgitation, area/pattern of jet (wrap around atrium) and effect on PV flow pattern.
- Assess TV function. If a repair/annuloplasty ring is performed mild residual TR ideal.
- Ensure that there is no resulting stenosis at the level of either AV valve if these have been repaired.
- SV ASD: Confirm appropriate drainage of PVs into the LA without narrowing of PV/SVC/SVC baffle/SVC-RA appendage anastomosis. PV flow should be pulsatile and low velocity.
- CS ASD: In patients without an LSVC, confirm closure of the CS. In those with an LSVC, the CS drains into the RA and the CS appears normal in the ME 2C view.
References/Suggested Reading:
- Operative Techniques in Thoracic and Cardiovascular Surgery series. Elsevier Inc.
- Seminars in Thoracic and Cardiovascular Surgery series. Pediatric Cardiac Surgery Annual. Elsevier Inc.
- Echocardiography for Pediatric and Congenital heart disease. Lai W, Mertens L, Cohen M, Geva T (eds), Wiley-Blackwell 2009
- Guidelines for Performing a Comprehensive Transesophageal Echocardiographic Examination: Recommendations from the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists. Hahn RT, Abraham T, Adams MS et al. J Am Soc Echocardiogr 2013:26:921-64.
- Echocardiographic assessment of atrial septal defects. Burch TM, Mizuguchi KA, DiNardo JA. Anesth Analg. 2012 Oct;115(4):772-5
Addendum 1–
TEE views to visualize ASDs
The following are the most commonly used TEE views to assess ASDs with arrows demonstrating where the defect is typically visualized. On some views additional arrows point to additional structures that should be specifically examined such as the anterior leaflet of the mitral valve for a cleft.
(Modified with permission from Table 10 in Guidelines for Performing a Comprehensive Transesophageal Echocardiographic Examination: Recommendations from the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists. Hahn RT, Abraham T, Adams MS et al. J Am Soc Echocardiogr 2013:26:921-64.
Elsevier, September 2013)